Abstract
A number of vascular risk factors (VRFs) have been reported to be associated with idiopathic normal-pressure hydrocephalus (iNPH), but it remains unclear whether these VRFs are related to patient outcomes after shunt surgery. Therefore, we investigated the risk factors for unfavourable outcomes after shunt surgery in iNPH patients using two samples from Tohoku University Hospital and from a multicentre prospective trial of lumboperitoneal (LP) shunt surgery for patients with iNPH (SINPHONI-2). We enrolled 158 iNPH patients. We compared the prevalence of VRFs and clinical measures between patients with favourable and unfavourable outcomes and identified predictors of unfavourable outcomes using multivariate logistic regression analyses. The presence of hypertension, longer disease duration, more severe urinary dysfunction, and a lower Evans’ index were predictors of unfavourable outcomes after shunt surgery. In addition, hypertension and longer disease duration were also predictors in patients with independent walking, and a lower Evans’ index was the only predictor in patients who needed assistance to walk or could not walk. Our findings indicate that hypertension is the only VRF related to unfavourable outcomes after shunt surgery in iNPH patients. Larger-scale studies are needed to elucidate the reason why hypertension can affect the irreversibility of symptoms after shunt placement.
Similar content being viewed by others
Introduction
Normal-pressure hydrocephalus (NPH) is a syndrome associated with dilated ventricles and is characterized by gait disturbance, cognitive impairment, and urinary dysfunction1. NPH is divided into two groups, i.e., idiopathic NPH (iNPH), which has an insidious onset of unknown cause, and secondary NPH, which is caused by a disease or event such as subarachnoid haemorrhage, meningitis, cerebral contusion, or brain tumour. The early and accurate diagnosis of iNPH is becoming increasingly important because iNPH has a high prevalence in the elderly population and has been shown to be treatable with cerebrospinal fluid (CSF) shunt surgery2,3,4. However, older age is associated with a higher rate of comorbidities, which makes surgery and perioperative management more complicated. Therefore, we need to carefully determine the surgical indications for patients with iNPH not only to reduce the frequency of complications but also to ensure that we perform shunt surgery only in patients who are expected to benefit from it.
Hypertension is one of the most common risk factors for iNPH5,6,7. Other vascular risk factors (VRFs), such as diabetes mellitus and hyperlipidaemia, have also been reported to be associated with iNPH8. Although the actual pathophysiology of iNPH remains unclear, these studies indicate that an alteration in CSF dynamics due to vascular dysfunction may be related to the pathogenesis of iNPH. On the other hand, in the small number of studies that have reported on whether VRFs are associated with outcomes after shunt surgery6,9,10,11, the results have been inconsistent. Moreover, hypertension and diabetes mellitus have been reported to play integral roles not only in cerebrovascular diseases (CVDs) but also in the pathogenesis of Alzheimer’s disease (AD)12,13,14. Previous studies performing cortical biopsy for patients with iNPH have reported that AD pathology was present in 25–67.6% of patients with iNPH and was related to worse baseline cognitive performance and diminished postoperative outcomes in patients with iNPH15,16,17. Whether VRFs are actually related to the pathogenesis of iNPH should be reconsidered.
The primary purpose of this study was to investigate risk factors for unfavourable outcomes after shunt surgery and whether VRFs are associated with shunt responsiveness in patients with iNPH. The second purpose was to examine whether these risk factors are different between patients with relatively milder and more severe gait disturbance. In the early and middle stages of AD, abnormal gait has rarely been observed18. It is assumed that there would be a group of iNPH patients with more severe cognitive impairment relative to their walking performance due to a combination of AD and iNPH pathologies. Moreover, these patients would have poor postoperative outcomes because the AD pathology potentially contributes to the irreversibility of cognitive symptoms after shunt surgery15,17,19. If VRFs are more closely related to AD pathology than to iNPH pathology, relatively more severe cognitive impairments at baseline and unfavourable postoperative outcomes would be correlated with a high prevalence of VRFs in iNPH patients with relatively milder gait disturbances. We believe that it is important to investigate those associations to improve the postoperative outcomes of shunt surgery in patients with iNPH and to consider the diversity of its neuropathology. For these purposes, we analysed two samples, consisting of participants from Tohoku University Hospital and from a multicentre prospective trial of lumboperitoneal (LP) shunt surgery for patients with iNPH (SINPHONI-2)4.
Methods
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Tohoku University Hospital (approval numbers: 2006-195, 2010-505, and 2020-1-285). Written informed consent was obtained from the patients and their families on the first admission.
SINPHONI-2 was conducted following the Guidelines for Good Clinical Practice and the Declaration of Helsinki. An independent committee monitored all the clinical data, imaging data, data related to safety issues, and protocol compliance through a web-based case report system. The study protocol was approved by the institutional review board at each site (see the SINPHONI-2 study centres below), and all patients or their representatives (if the patients could not understand the contents of the study) provided written informed consent before entry into the study.
Participants from Tohoku University Hospital
One hundred forty-seven (61 women/86 men) consecutive patients with iNPH who were admitted to Tohoku University Hospital were enrolled between December 2006 and November 2016. All patients fulfilled the following criteria and underwent shunt surgery regardless of the response to the CSF tap test: (1) > 60 years of age; (2) gait disturbance, cognitive impairment, and/or urinary disturbance; (3) both ventricular dilation (Evans’ index > 0.3) and high convexity and medial subarachnoid space tightness on coronal MRI; (4) CSF pressure < 200 mmH2O with normal CSF cell counts and protein levels; (5) lack of a previous history of conditions that might cause ventricular dilation; and (6) the absence of other diseases that may account for such symptoms.
The choice of operative procedure, i.e., ventriculoperitoneal (VP) or LP shunt implantation, was determined according to the patient’s wishes and condition, such as the presence of spinal canal stenosis. The operations were conducted at Tohoku University Hospital or Kohnan Hospital. VP shunt implantation was conducted using a Codman-Hakim programmable valve with a Siphon-Guard (Codman and Shurtleff, Integra LifeSciences Corporation, Plainsboro, NJ, USA), and LP shunt implantation was conducted using a Codman-Hakim programmable valve with a Siphon-Guard or a Strata NSC adjustable-pressure valve with a Siphon-Control Device (Medtronic Inc., Minneapolis, MN, USA). Postoperatively, if clinical improvement was insufficient, pressure adjustments were made repeatedly until the optimal pressure for the patient was attained.
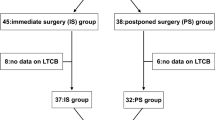
Figure 1-a shows the flow chart of patient selection. Eighty-two of the initial set of patients were re-evaluated approximately 1 year (12 ± 1 months) after shunt surgery. The remaining 65 patients were not reassessed for various reasons. Moreover, four of the re-evaluated patients were excluded from the analysis because of complications that interfered with the postoperative evaluation of iNPH symptoms. Consequently, 78 patients were included in the following analyses.
SINPHONI-2 study
Ninety-three (43 women/50 men) patients with iNPH were enrolled from 20 neurological and neurosurgical centres in Japan between March 2010 and October 2011. The inclusion criteria were (1) age between 60 and 85 years; (2) gait disturbance, cognitive impairment, and/or urinary disturbance; (3) both ventricular dilation (Evans’ index > 0.3) and high-convexity and medial subarachnoid space tightness on coronal MRI; (4) CSF pressure < 200 mmH2O with normal CSF cell counts and protein levels; (5) lack of a previous history of conditions that might cause ventricular dilation; (6) the absence of other diseases that may account for such symptoms; (7) a normal Queckenstedt’s test; and (8) the absence of severe vertebral degenerative diseases or spinal canal stenosis as shown on plain radiographs or MRI. Figure 1-b shows the flow chart for patient selection. Forty-nine (29 women/20 men) of the initial patients were randomly assigned to undergo LP shunt implantation within 1 month of randomization, and the remaining 44 (14 women/30 men) patients were assigned to delayed LP shunt implantation 3 months after randomization. All participants in both SINPHONI-2 groups underwent a tap test after randomization and were followed up until 12 months after shunt surgery. Consequently, 80 patients in both groups, except for three patients recruited from Tohoku University Hospital, were included in the following analyses. The details of the study were previously described4.
Clinical assessments
In both studies, the patients underwent clinical assessment at baseline prior to both CSF removal and shunt implantation and were reassessed approximately 1 year after shunt implantation. We used the modified Rankin Scale (mRS) to define shunt responsiveness20. The mRS has been commonly used for evaluating physical disability or dependence in activities of daily living in acute stroke trials and was adopted for evaluating outcomes of shunt surgery in multicentre studies of iNPH3,4. In the current study, a favourable outcome of shunt implantation was defined as an improvement by one or more points on the mRS at the 1-year follow-up after shunt surgery. The severity of the triad was assessed using the idiopathic normal-pressure hydrocephalus grading scale (iNPHGS)21, and the patients were classified into the following two groups using the iNPHGS gait subscore: (1) the preserved walking performance group (iNPHGS gait subscore ≤ 2, i.e., patients who could walk independently) and (2) the reduced walking performance group (iNPHGS gait subscore ≥ 3, i.e., patients who needed assistance to walk or who could not walk).
We administered the timed up-and-go test (TUG) to assess gait function22. The completion time was used as the score. Patients who could not rise from an armchair and/or walk safely and independently were not assessed. Moreover, we administered the following neuropsychological measures: (1) the Mini-Mental State Examination (MMSE), whose total score was used to assess general cognitive function23; (2) the Frontal Assessment Battery (FAB), whose total score was used to assess executive function24; and (3) the Trail Making test A (TMT-A), whose completion time was used to assess psychomotor speed25;if a patient could not complete the task within the time limit of 420 s, the patient was given a score of 420 s.
Vascular risk factors
We investigated the VRFs in each patient. The criteria for these factors were as follows: (1) hypertension: systolic blood pressure ≥ 140 and/or diastolic blood pressure ≥ 90 mmHg, or use of antihypertensive drugs; (2) diabetes mellitus: fasting plasma glucose level ≥ 126 mg/dl and haemoglobin A1c level ≥ 6.5% or usage of hypoglycaemic drugs; (3) hyperlipidaemia; plasma low-density lipoproteins ≥ 140 mg/dl and/or triglycerides ≥ 150 mg/dl or use of a lipid-lowering drug; (4) smoking: current or past smoking; and (5) ischaemic stroke: a history of cerebral infarction (lacunar stroke, atherothrombotic stroke, cardiogenic embolic stroke, and/or haemodynamic stroke) or transient ischaemic attack or the presence of ischaemic lesions on presurgical MRI. We prospectively checked these data except for the presence of ischaemic lesions on presurgical MRI (retrospectively). In the present study, periventricular hyperintensity and deep white matter hyperintensity were not assessed to avoid overdetection of ischaemic lesions.
Statistical analyses
The demographic data, the prevalence of VRFs, and clinical measures at baseline were compared in all participants and in each walking performance group as follows: (1) the participants from Tohoku University Hospital versus SINPHONI-2; and (2) the patients with favourable versus unfavourable outcomes. Furthermore, to discuss the differences in the results between our study and Nakajima et al.’s previous studies, we compared the prevalence of each VRF that was significantly different between the patients with favourable and unfavourable outcomes among patients with the same mRS score (grade 1–2, grade 3, or grade 4)9.
We used the chi-square test to compare the sex distribution, the prevalence of VRFs, the operative procedure, and shunt responsiveness between groups. Student’s t test was used for age, educational attainment, disease duration, Evans’ index, and the scores of neuropsychological and gait tests. The Mann–Whitney U test was used for the mRS score and the iNPHGS total and subscores. To evaluate the changes in clinical measures after shunt implantation among only patients with favourable or unfavourable outcomes, the paired Student’s t test was used to compare the scores of neuropsychological and gait tests, and the Wilcoxon signed-ranked test was used to compare the mRS score and the iNPHGS total and subscores.
Finally, we performed multivariate logistic regression analysis by the forced-entry method to identify the predictors of unfavourable outcome in all participants and in each walking performance group. Each independent variable included in these analyses was selected when its p value for comparisons between patients with favourable and unfavourable outcomes was below 0.1. Multicollinearity among independent variables was identified based on the variance inflation factor (VIF).
Statistical analyses were performed with SPSS statistics for version 25.0 (IBM, Armonk, New York). A p value < 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of participants at baseline
The demographic data and the results of clinical measures at baseline are shown in Table 1. We failed to investigate educational attainment in 12 patients and disease duration in one patient. We did not use the Evans’ index of one patient because of the presence of cavum vergae. In addition, we lost the Evans’ index of one patient from the SINPHONI-2 trial due to data collection failure. Two patients did not complete the FAB, and 15 patients did not complete the TMT-A because of severe cognitive impairments or refusal. Ten patients did not undergo the TUG because they could not rise from the armchair and/or walk safely and independently. Although we could check the presence of ischaemic lesions on presurgical MRI in all patients from Tohoku University Hospital, we could not check this in 23 patients from SINPHONI-2 retrospectively.
The analyses targeting all participants demonstrated that the participants from Tohoku University Hospital had a significantly longer disease duration, lower educational attainment, greater Evans’ index, lower mRS scores, shorter TUG completion time, higher MMSE total scores, and a higher prevalence of hyperlipidaemia than those from SINPHONI-2. In addition, the participants from Tohoku University Hospital tended to show lower iNPHGS gait subscores, lower total FAB scores, and poorer shunt response than those from SINPHONI-2. There was no apparent difference in age, sex ratio, iNPHGS cognition or urination subscore or total score, TMT-A score, or the prevalence of any VRF except for hyperlipidaemia between the participants from Tohoku University Hospital and from SINPHONI-2.
In the preserved walking performance group, the participants from Tohoku University Hospital had a significantly longer disease duration, greater Evans’ index, and shorter TUG completion time than those from SINPHONI-2. The participants from Tohoku University Hospital also tended to show higher iNPHGS gait subscores and lower educational attainment than those from SINPHONI-2. There was no apparent difference in age, sex ratio, mRS score, iNPHGS cognition or urination subscore or total score, the score of any neuropsychological test we administered, or the prevalence of any VRF between the preserved walking performance participants from Tohoku University Hospital and SINPHONI-2.
In the reduced walking performance group, the participants from Tohoku University Hospital had significantly lower educational attainment and higher MMSE total scores than those from SINPHONI-2. In addition, there tended to be more female participants from Tohoku University Hospital than from SINPHONI-2. There was no apparent difference in age, Evans’ index, mRS score, any iNPHGS subscore or total score, FAB score, TMT-A score, TUG completion time, or the prevalence of any VRF between the reduced walking performance participants from Tohoku University Hospital and SINPHONI-2.
Although there was no significant difference in shunt surgery outcomes between the participants from each walking performance group, the proportion of patients with favourable outcomes from Tohoku University Hospital tended to be lower than that from SINPHONI-2 (Tohoku University Hospital: 47.4% (37/78), SINPHONI-2: 62.5% (50/80), p = 0.057). Supplementary Table 1 lists the adverse events during the 1-year follow-up period at Tohoku University Hospital. These patients had fewer serious adverse events (defined as those resulting in hospitalization, prolongation of hospitalization, and significant disability) than the participants from SINPHONI-24.
Clinical measures and the VRFs associated with shunt responsiveness
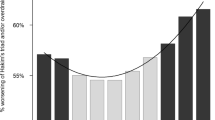
The differences in demographics and clinical measures between the patients with favourable and unfavourable outcomes are shown in Table 2. The analyses targeting all participants demonstrated that the participants with unfavourable outcomes showed a significantly longer disease duration, lower Evans’ index, and a higher prevalence of hypertension than those with favourable outcomes. In addition, the median iNPHGS urination subscore of patients with unfavourable outcomes tended to be higher than that of patients with favourable outcomes. In the preserved walking performance group, the prevalence of hypertension in patients with unfavourable outcomes was significantly higher than in those with favourable outcomes (Fig. 2-a). In addition, patients with unfavourable outcomes tended to show a longer disease duration, lower total MMSE and FAB scores, and a higher prevalence of diabetes mellitus than those with favourable outcomes. In the reduced walking performance group, patients with unfavourable outcomes showed a significantly lower Evans’ index and a higher prevalence of a history of ischaemic stroke than those with favourable outcomes (Fig. 2-a). Moreover, the median iNPHGS urination subscore of patients with unfavourable outcomes tended to be higher than that of patients with favourable outcomes.
The prevalence of hypertension and ischaemic stroke history. (a) Patients with iNPHGS gait subscores of 2 or below and with iNPHGS gait subscores of 3 or above. (b) Patients with an mRS grade 1 or 2, grade 3, and grade 4. iNPHGS idiopathic normal-pressure hydrocephalus grading scale, mRS modified Rankin Scale. *p < 0.05, **p < 0.005, ***p < 0.001.
The prevalences of hypertension and ischaemic stroke history in patients with each mRS score are shown in Fig. 2-b. Among the patients with mRS grade 1 or 2, those with unfavourable outcomes had a significantly higher prevalence of hypertension than those with favourable outcomes (p < 0.001). Among the patients with mRS grade 3, the prevalence of hypertension in patients with unfavourable outcomes tended to be higher than that in patients with favourable outcomes (p = 0.057). By contrast, among the patients with mRS score 4, the prevalence of hypertension in patients with unfavourable outcomes was significantly lower than that in those with favourable outcomes (p = 0.003). Among the patients with each mRS score, there was no significant difference in the prevalence of ischaemic stroke history between patients with favourable and unfavourable outcomes (mRS grade 1 or 2, p = 0.514; mRS grade 3, p = 0.589; and mRS grade 4, p = 0.100).
Changes in clinical measures after shunt implantation
The changes in clinical measures after shunt implantation are shown in Table 3 (all participants and each working performance group) and Supplementary Table 2 (each sample). The analyses targeting all participants demonstrated that the participants with favourable outcomes showed significant improvements in iNPHGS sub- and total scores, the scores of all neuropsychological tests, and TUG completion time, whereas participants with unfavourable outcomes showed significant improvements only in iNPH gait, urination sub- and total scores, and TUG completion time. In the preserved walking performance group, patients with favourable outcomes showed significant improvements in mRS score, iNPHGS sub- and total scores, TUG completion time, and scores of all neuropsychological tests except for TMT-A, whereas patients with unfavourable outcomes did not show significant improvement in any clinical measures we administered except for TUG completion time and iNPHGS total scores. In the reduced walking performance group, patients with favourable outcomes showed significant improvements in mRS score, iNPHGS sub- and total scores, TUG completion time, and the scores of all neuropsychological tests except for MMSE, whereas patients with unfavourable outcomes showed significant improvement only in iNPHGS gait sub- and total scores and TUG completion time.
Predictors of unfavourable outcomes after shunt surgery
The results of multivariate logistic analyses are shown in Table 4. Multicollinearity was not found in any of the analyses. For the analysis targeting all participants, disease duration, the iNPHGS urination subscore, the prevalence of hypertension, and Evans’ index were selected. All of these variables were significant risk factors for unfavourable outcomes after shunt surgery. In the preserved walking performance group, disease duration, total MMSE score (VIF = 1.816), FAB score (VIF = 1.877), and the prevalence of hypertension and diabetes mellitus (VIF = 1.099) were selected. Among these variables, disease duration and hypertension were significant risk factors for unfavourable outcomes after shunt surgery. In the reduced walking performance group, the iNPHGS urination subscore (VIF = 1.027), the prevalence of ischaemic stroke history (VIF = 1.059), and Evans’ index were selected for the analysis. Of these variables, Evans’ index was the only significant risk factor for unfavourable outcomes after shunt surgery.
Discussion
Predictors of unfavourable outcomes in iNPH patients
In the analyses targeting all participants, we showed that the presence of hypertension, more severe urinary dysfunction evaluated by the iNPHGS urination subscore, relatively smaller lateral ventricles for hydrocephalus measured using Evans’ index, and longer disease duration were predictors of unfavourable outcomes after shunt surgery. In our results, hypertension was the only VRF that could predict shunt responsiveness. In the subgroup analyses, hypertension was more associated with iNPH patients with independent walking than those who needed assistance to walk or could not walk.
A few studies have reported whether VRFs are associated with outcomes after shunt surgery6,9,10,11, but their results are inconsistent. Boon et al. demonstrated that the proportion of shunt responders among iNPH patients with CVD was significantly lower than that among iNPH patients without CVD6. Andrén et al. reported that the presence of vascular comorbidity had almost no negative impact on the outcome 2–6 years after shunt surgery, but patients with hypertension and/or a history of stroke showed a less favourable progression on the self-assessed mRS only 6 years after shunt surgery10. In the study by Klinge et al., the presence of VRFs was not correlated with the magnitude of improvement after shunt surgery11. Taking mRS score as a measure of physical disability, including gait disturbance, the patients’ severity in Boon et al.’s study was near that among patients in our study who needed assistance to walk or could not walk, and the patients’ severity in Andrén et al.’s study was almost equivalent to that of patients in our study with independent walking. As with our study, Boon et al.’s and Andrén et al.’s studies revealed an association between VRFs and poor outcomes after shunt surgery. However, our study did not reveal any association between hypertension and long-term outcomes, and Andrén et al. did not find any association between hypertension and short-term outcomes.
In addition, the subgroup analyses of patients with independent walking revealed that the MMSE and FAB total scores in patients with unfavourable outcomes tended to be lower than in those with favourable outcomes, although these findings were not statistically significant. These results were coincident with the expectations derived from our hypothesis that hypertension might be more closely related to AD than to iNPH pathology. However, Nakajima et al. reported that patients with mRS grade 3 at baseline showed an association between comorbid AD and unfavourable outcomes9. Of these patients, those who had unfavourable outcomes had a significantly lower prevalence of hypertension than those who had favourable outcomes. These findings are incompatible with our results and hypothesis, even though the diagnostic process for comorbid AD used by Nakajima et al. was uncertain. Interestingly, we observed the same improvement effect of hypertension on iNPH symptoms after shunt surgery that Nakajima et al. did, although only in patients with mRS grade 4 at baseline in our study. Hypertension seems to play a bidirectional role in shunt responsiveness, so the effect of hypertension on shunt responsiveness may be offset, depending on the severity of physical disability in patients with iNPH. Although the mRS is a well-validated and reliable tool for evaluating activities of daily life or physical disability, interobserver studies closest in design to large-scale clinical trials demonstrate potentially significant interobserver variability26. Large-scale cohort studies with improved evaluations of activities of daily life and/or physical disability are needed to explain these discrepancies in results.
Previous studies have reported that hypertension is one of the common risk factors for the pathogenesis of iNPH5,6,7,8. However, the prevalence of hypertension in our patients was lower than that in septuagenarian men (74.7–81.4%) and women (69.2–72.3%) between 2010 and 2016 in Japan, except among patients with independent walking who had unfavourable outcomes after shunt surgery27. Previous studies have also indicated a lower prevalence of hypertension in patients with iNPH, except in Israelsson et al.’s study6,8,9,10,11. It should be reconsidered whether hypertension is actually related to the pathogenesis of iNPH. The glymphatic and intramural periarterial drainage pathways, which play a crucial role in maintaining brain interstitial fluid homeostasis and washing out waste products, have recently drawn attention not only in AD but also in iNPH studies28,29,30,31,32. It is thought that these pathways are driven by pulsations of the arterial wall33. A recent rat study revealed that hypertension increases CSF backflow and thereby reduces CSF net flow in the perivascular space34. Although impairments in these pathways related to hypertension may be associated not only with the decline in amyloid beta clearance from the central nervous system but also with ventriculomegaly in iNPH, our and Nakajima et al.’s results suggest the possibility that comorbid hypertension facilitates the drainage of CSF through an inserted catheter or through the perivascular space after shunt surgery in some iNPH patients.
In the present study, more severe urinary dysfunction was also associated with unfavourable outcomes after shunt surgery in patients with iNPH. To the best of our knowledge, no previous studies have demonstrated an association between urinary dysfunction and shunt responsiveness in patients with iNPH. It is known that patients with iNPH have urge and functional urinary incontinence35. However, urinary dysfunction is common in elderly individuals, and urge and functional urinary incontinence are also observed in patients with other neurological diseases, such as cerebrovascular disease, AD, or Parkinson’s disease36. Therefore, there was a possibility that some iNPH patients with severe urinary dysfunction had comorbid neurological disease, which led to unfavourable outcomes after shunt surgery in the iNPH patients.
A longer disease duration was also related to unfavourable outcomes after shunt surgery in patients with iNPH. This finding is consistent with previous studies. Kimura et al. and Vakili et al. reported that a longer symptom duration was associated with less improvement in mRS at 6 months or 1 year postoperatively37,38. In addition, in our study, a longer disease duration was more associated with iNPH patients with independent walking than with those who needed assistance to walk or could not walk. We speculate that this discrepancy between the two groups might arise from some comorbid neurological disease in some patients with independent walking, such as AD, which does not result in severe gait disturbance in the early and moderate stages of the disease. If these patients might have asymptomatic ventriculomegaly with features of iNPH on MRI, their symptoms might be not mainly due to iNPH but due to comorbid neurological diseases2.
Having fairly small lateral ventricles at baseline was also associated with an unfavourable outcome after shunt surgery. Moreover, in the subgroup analyses, this finding was more associated with iNPH patients who needed assistance to walk or could not walk than those with independent walking. To the best of our knowledge, there has been no report of a significant association between ventricular size and symptom severity at baseline or between ventricular size at baseline and shunt responsiveness in patients with iNPH. However, several previous studies have reported that a reduction in ventricular size after shunt implantation was positively associated with the magnitude of clinical improvement in patients with iNPH39,40. The relatively small lateral ventricles in hydrocephalus at baseline may reflect low elasticity and plasticity of the brain parenchyma. However, a significant association between ventricular size at baseline and shunt responsiveness was not observed in the patients with independent walking. One possible reason is that ventricular dilation was caused not only by iNPH-related pathology but also by AD- and/or CVD-related pathology. Because of these conflicting factors influencing reversibility after shunt surgery, ventricular size at baseline could not predict shunt responsiveness in patients with independent walking.
Participants from Tohoku University Hospital and SINPHONI-2
Among the participants from Tohoku University Hospital, more could walk independently and fewer needed assistance to walk or could not walk than among the participants from SINPHONI-2. In addition, patients from Tohoku University showed shorter TUG completion times than those from SINPHONI-2. Although the combination of the two samples allowed us to investigate iNPH patients with milder to more severe gait disturbances, it should be noted that the results in patients with independent walking might have been easily influenced by the measurement bias related to the single-hospital nature of the data. Moreover, the disease duration of the participants from Tohoku University Hospital was significantly longer than that from SINPHONI-2. Although these findings might be true, it might be that the evaluators in Tohoku University Hospital tended to take a more detailed medical history than those in the other institutes that participated in SINPHONI-2.
The participants from Tohoku University Hospital were less likely to have favourable outcomes than those from SINPHONI-2, although this finding was not statistically significant. The quality of shunt surgery seemed not to be associated with poorer outcomes of shunt surgery in Tohoku University Hospital because the number of serious adverse events was lower in the participants from Tohoku University Hospital than in the participants from SINPHONI-2. One possible reason for the poorer outcomes in the Tohoku University Hospital cohort is that these participants had a longer disease duration than those from SINPHONI-237,38. Another possible reason is that evaluators at Tohoku University Hospital could have tended to overestimate symptom severity and/or underestimate the improvements in symptoms after shunt surgery when evaluated using severity scales. Among participants with independent walking, the mean TUG completion time in those from Tohoku University Hospital was significantly shorter than that in SINPHONI-2 patients, whereas the median iNPHGS gait subscore in participants from Tohoku University Hospital tended to be greater. In addition, the improvements in cognitive deficits as assessed by the MMSE and FAB in participants from Tohoku University Hospital were more marked than they were in the SINPHONI-2 groups, even though the magnitude of improvements in cognitive deficits as measured by the iNPHGS cognition subscore was equivalent between the two groups (Supplementary Table 2).
Limitation
The present study has several limitations. First, we did not evaluate CSF biomarkers for AD, perform amyloid imaging, or test memory function. Therefore, we cannot state with certainty that hypertension was associated with the presence of AD pathology in patients with independent walking. Second, the results in patients with independent walking might have been influenced by measurement bias because almost 60% of these patients were recruited from Tohoku University Hospital. Third, we were able to check the presence of ischaemic lesions on presurgical MRI only for approximately 70% of the participants from SINPHONI-2 but for all the participants from Tohoku University Hospital. Therefore, the prevalence of a history of ischaemic stroke was more influenced by the trends in the participants from Tohoku University Hospital.
Conclusions
Our study demonstrated that hypertension was the only VRF that could predict unfavourable outcomes after shunt surgery in patients with iNPH. In addition, more severe urinary dysfunction, relatively smaller lateral ventricles in hydrocephalus, and longer disease duration were also predictors. Larger-scale studies of comorbidities, including AD and CSF dynamics, are needed to elucidate the reason why hypertension is related to the irreversibility of symptoms after shunt placement.
Data availability
The datasets used and/or analysed during the current study are not publicly available due to participant’s privacy protections but are available from the corresponding author upon reasonable request.
References
Adams, R. D., Fisher, C. M., Hakim, S., Ojemann, R. G. & Sweet, W. H. Symptomatic occult hydrocephalus with “normal” cerebrospinal-fluid pressure. A treatable syndrome. N. Engl. J. Med. 273, 117–126 (1965).
Iseki, C. et al. Asymptomatic ventriculomegaly with features of idiopathic normal pressure hydrocephalus on MRI (AVIM) in the elderly: A prospective study in a Japanese population. J. Neurol Sci. 277, 54–57 (2009).
Hashimoto, M., Ishikawa, M., Mori, E. & Kuwana, N. Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res. 7, 18 (2010).
Kazui, H., Miyajima, M., Mori, E., Ishikawa, M., SINPHONI-2 Investigators. Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): An open-label randomised trial. Lancet Neurol. 14, 585–594 (2015).
Graff-Radford, N. R. & Godersky, J. C. Idiopathic normal pressure hydrocephalus and systemic hypertension. Neurology 37, 868–871 (1987).
Boon, A. J. et al. Dutch normal-pressure hydrocephalus study: The role of cerebrovascular disease. J. Neurosurg. 90, 221–226 (1999).
Malm, J. et al. Influence of comorbidities in idiopathic normal pressure hydrocephalus—Research and clinical care. A report of the ISHCSF task force on comorbidities in INPH. Fluids Barriers CNS. 10, 22 (2013).
Israelsson, H., Larsson, J., Eklund, A. & Malm, J. Risk factors, comorbidities, quality of life, and complications after surgery in idiopathic normal pressure hydrocephalus: Review of the INPH-CRasH study. Neurosurg. Focus 49, E8 (2020).
Nakajima, M. et al. Background risk factors associated with shunt intervention for possible idiopathic normal pressure hydrocephalus: A Nationwide Hospital-Based Survey in Japan. J. Alzheimers Dis. 68, 735–744 (2019).
Andrén, K. et al. Long-term effects of complications and vascular comorbidity in idiopathic normal pressure hydrocephalus: A quality registry study. J. Neurol. 265, 178–186 (2018).
Klinge, P., Hellström, P., Tans, J., Wikkelsø, C., European iNPH Multicentre Study Group. One-year outcome in the European multicentre study on iNPH. Acta Neurol. Scand. 126, 145–153 (2012).
Breteler, M. M. Vascular risk factors for Alzheimer’s disease: An epidemiologic perspective. Neurobiol. Aging 21, 153–160 (2000).
de la Torre, J. C. Cerebral hemodynamics and vascular risk factors: Setting the stage for Alzheimer’s disease. J. Alzheimers Dis. 32, 553–567 (2012).
Daugherty, A. M. Hypertension-related risk for dementia: A summary review with future directions. Semin. Cell Dev. Biol. 116, 82–89 (2021).
Hamilton, R. et al. Lack of shunt response in suspected idiopathic normal pressure hydrocephalus with Alzheimer disease pathology. Ann. Neurol. 68, 535–540 (2010).
Leinonen, V. et al. Cortical brain biopsy in long-term prognostication of 468 patients with possible normal pressure hydrocephalus. Neurodegener. Dis. 10, 166–169 (2012).
Kazui, H. et al. Association between high biomarker probability of Alzheimer’s disease and improvement of clinical outcomes after shunt surgery in patients with idiopathic normal pressure hydrocephalus. J. Neurol. Sci. 369, 236–241 (2016).
Day, G. S. et al. Differentiating cognitive impairment due to corticobasal degeneration and Alzheimer disease. Neurology 88, 1273–1281 (2017).
Bådagård, H., Braun, M., Nilsson, D., Stridh, L. & Virhammar, J. Negative predictors of shunt surgery outcome in normal pressure hydrocephalus. Acta Neurol. Scand. 141, 219–225 (2020).
van Swieten, J. C., Koudstaal, P. J., Visser, M. C., Schouten, H. J. & van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19, 604–607 (1988).
Kubo, Y. et al. Validation of grading scale for evaluating symptoms of idiopathic normal-pressure hydrocephalus. Dement. Geriatr. Cogn. Disord. 25, 37–45 (2008).
Podsiadlo, D. & Richardson, S. The timed ‘“Up & Go”’: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39, 142–148 (1991).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. ‘“Mini-mental state”’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Dubois, B., Slachevsky, A., Litvan, I. & Pillon, B. The FAB: A frontal assessment battery at bedside. Neurology 55, 1621–1626 (2010).
Reitan, R. Validity of the trail making test as an indicator of organic brain damage. Percept. Mot. Skills 8, 271–276 (1958).
Quinn, T. J., Dawson, J., Walters, M. R. & Lees, K. R. Reliability of the modified Rankin Scale: A systematic review. Stroke 40, 3393–3395 (2009).
Hisamatsu, T. & Miura, K. Epidemiology and control of hypertension in Japan: A comparison with Western countries. J. Hum. Hypertens. https://doi.org/10.1038/s41371-021-00534-3 (2021). Online ahead of print.
Iliff, J. J. et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci. Transl. Med. 4, 147ra111 (2012).
Carare, R. O., Hawkes, C. A. & Weller, R. O. Afferent and efferent immunological pathways of the brain. Anatomy, function and failure. Brain Behav. Immun. 36, 9–14 (2014).
Weller, R. O., Djuanda, E., Yow, H. Y. & Carare, R. O. Lymphatic drainage of the brain and the pathophysiology of neurological disease. Acta Neuropathol. 117, 1–14 (2009).
Reeves, B. C. et al. Glymphatic system impairment in Alzheimer’s disease and idiopathic normal pressure hydrocephalus. Trends Mol. Med. 26, 285–295 (2020).
Ringstad, G., Vatnehol, S. A. S. & Eide, P. K. Glymphatic MRI in idiopathic normal pressure hydrocephalus. Brain 140, 2691–2705 (2017).
Iliff, J. J. et al. Cerebral arterial pulsation drives paravascular CSF-interstitial fluid exchange in the murine brain. J. Neurosci. 33, 18190–18199 (2013).
Mestre, H. et al. Flow of cerebrospinal fluid is driven by arterial pulsations and is reduced in hypertension. Nat. Commun. 9, 4878 (2018).
Sakakibara, R. et al. Correlation of right frontal hypoperfusion and urinary dysfunction in iNPH: A SPECT study. Neurourol. Urodyn. 31, 50–55 (2012).
Erdem, K. & Chu, F. M. Management of overactive bladder and urge urinary incontinence in the elderly patient. Am J Med. 119, 29–36 (2006).
Kimura, T. et al. Preoperative predictive factors of short-term outcome in idiopathic normal pressure hydrocephalus. World Neurosurg. 151, E399–E406 (2021).
Vakili, S. et al. Timing of surgical treatment for idiopathic normal pressure hydrocephalus: Association between treatment delay and reduced short-term benefit. Neurosurg. Focus. 41, E2 (2016).
Neikter, J. et al. Ventricular volume is more strongly associated with clinical improvement than the Evans index after shunting in idiopathic normal pressure hydrocephalus. AJNR. Am. J. Neuroradiol. 41, 1187–1192 (2020).
Hiraoka, K. et al. Changes in the volumes of the brain and cerebrospinal fluid spaces after shunt surgery in idiopathic normal-pressure hydrocephalus. J. Neurol. Sci. 296, 7–12 (2010).
Acknowledgements
We thank the patients and their families for their participation in this study. This work was supported by Grants from JSPS KAKENHI (Grant Numbers JP16K01447 and JP20K11202) to SK and Health Labour Sciences Research (Grant Numbers 20GB1002 and 20GC1008) to KS. SINPHONI-2 was supported in part by Johnson & Johnson and Nihon Medi-Physics. The funding sources had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. SINPHONI-2 study centres: Rakuwakai Otowa Hospital, Kyoto, Japan; Tohoku University Graduate School of Medicine, Sendai, Japan; Juntendo University Graduate School of Medicine, Tokyo, Japan; Noto General Hospital, Nanao, Japan; Osaka Medical Collage, Takatsuki, Japan; Nishinomiya Kyoritsu Neurosurgical Hospital, Nishinomiya, Japan; Hamamatsu Medical Centre, Hamamatsu, Japan; Shinko Hospital, Kobe, Japan; Osaka University Graduate School of Medicine, Suita, Japan; Tokyo Kyosai Hospital, Tokyo, Japan; Yokohama Minami Kyosai Hospital, Yokohama, Japan; Okayama University Graduate School of Medicine, Okayama, Japan; Kumamoto Takumadai Rehabilitation Hospital, Kumamoto, Japan; Atsuchi Neurosurgical Hospital, Kagoshima, Japan; Tama-Hokubu Medical Centre, Higashimurayama, Japan; Kanazawa University Graduate School of Medicine, Kanazawa, Japan; Tama-Nanbu Regional Hospital, Tama, Japan; Dohtoh Neurosurgical Hospital, Kitami, Japan; Megumino Hospital, Eniwa, Japan; Tsudanuma Central General Hospital, Narashino, Japan.
Author information
Authors and Affiliations
Contributions
E.K. helped design the study at Tohoku University Hospital, acquired and analysed the data, and wrote the manuscript. S.K. helped design the study at Tohoku University Hospital, acquired and analysed the data, and edited the manuscript. N.K. and W.N. acquired and analysed the data from Tohoku University Hospital. M.S. and K.E. acquired the data from Tohoku University Hospital. M.I. and T.K. performed the shunt operation (for participants from Tohoku University Hospital). S.Y. and K.I. analysed the data from SINPHONI-2. H.K., M.M., M.I., and E.M. designed and supervised the SINPHONI-2 study. T.T. and F.T. helped supervise the study at Tohoku University Hospital. K.S. helped supervise the study at Tohoku University Hospital and edited the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
E.K., S.K., N.K., W.N., M.S., K.E., M.I., and T.K. have no competing interests to disclose. S.Y. received grants from the G-7 Scholarship Foundation, Taiju Life Social Welfare Foundation, and FUJIFILM Corporation and speaker honoraria from Fujifilm Medical Systems, Integra Japan, and Daiichi Sankyo, outside the submitted work. K.I. received funding for speaker honoraria from Nihon Medi-Physics. H.K. received funding for travel and/or speaker honoraria from Integra Japan, Nihon Medi-Physics, Ono Pharmaceutical, Pfizer, Eisai, Daiichi-Sankyo, Janssen Pharmaceutical, Takeda Pharmaceutical, Novartis Pharma and Medtronic Inc. and receives research support from MSD KK, Daiichi-Sankyo, Eisai, a Japan Society for the Promotion of Science Grant-in-Aid for Scientific Research, a Health Labour Sciences Research Grant, and the Japan Agency for Medical Research and Development. M.M. received funding for travel and/or speaker honoraria from Integra Japan, Nihon Medi-Physics, Medtronic, Novartis Pharma, Eisai and Daiichi-Sankyo. M.I. received speaker honoraria from Integra Japan, Nihon Medi-Physics, Medtronic and Eisai. E.M. received speaker honoraria from Eisai, Daiichi-Sankyo, Novartis Pharma, Integra Japan, Nihon Medi-Physics, Janssen Pharmaceutical, Medtronic, Otsuka, Tanabe-Mitsubishi, Ono, and Fujifilm Medical; served as a consultant for Lundbeck; and received research support from Eisai, Daiichi-Sankyo, Novartis Pharma, Tanabe-Mitsubishi, Fujifilm Medical, and the Ministry of Health, Labour and Welfare Japan. T.T., F.T., and K.S. have no competing interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kobayashi, E., Kanno, S., Kawakami, N. et al. Risk factors for unfavourable outcomes after shunt surgery in patients with idiopathic normal-pressure hydrocephalus. Sci Rep 12, 13921 (2022). https://doi.org/10.1038/s41598-022-18209-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18209-5
This article is cited by
-
Clinical improvements in temporospatial gait variables after a spinal tap test in individuals with idiopathic normal pressure hydrocephalus
Scientific Reports (2024)
-
Association between vascular risk factors and idiopathic normal pressure hydrocephalus: a Mendelian randomization study
Journal of Neurology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.