Abstract
During tumorigenesis, certain tissues are colonized by mutant clones with oncogenic driver mutations as precancer lesions. These mutations can facilitate clonal expansion and may contribute to malignant transformation. The molecular features of low-grade non-muscle invasive bladder cancer (NMIBC) and high-grade bladder cancer are so distinct that they are thought to follow different evolutionary tumorigenesis pathways. Although NMIBC accounts for most bladder tumors, the somatic mutation patterns in “precancer” urothelium of patients with NMIBC remain unclear. Here, we analyzed specimens of normal urothelium and bladder tumors from patients with low-grade and high-grade NMIBC and investigated the genomic evolution of the cancer. Somatic mutations were analyzed using 50 oncogene-targeted sequences and droplet digital polymerase chain reaction for TERT promoter mutations. Somatic mutations in TERT promoter, FGFR3, and CDKN2A were characteristically identified in the normal urothelium of patients with NMIBC. These mutations, consistently identified in both tumor and normal specimens, likely affect clonal expansion during the malignant transformation of NMIBC. Though larger samples and comprehensive study are warranted to confirm our results, the difference in mutational landscape of the precancerous urothelium of patients with bladder cancer could offer deeper understandings of genomic evolution in bladder tumorigenesis.
Similar content being viewed by others
Introduction
During aging, somatic mutations accumulate in normal cells, mainly due to DNA replication errors or genomic instability during cell division. The genomic evolution model of colorectal cancer1, in which the accumulation of somatic mutations in the normal epithelium, or early adenoma, drives clonal expansion and eventual malignant transformation, is well recognized. It is, therefore, important to perform genomic analysis in “precancer” epithelium and tumor tissues to gain a deeper understanding of genomic evolution involved in tumorigenesis. Recent technological developments in genomic sequencing have revealed the mutational landscape of various types of normal tissues, including colon2, liver3, esophagus4, epidermis5, bronchus6, blood cells7, and urothelium8,9, offering a deeper understanding of cancer-promoting factors in the normal epithelium.
Most bladder cancers are non-muscle invasive bladder cancers (NMIBCs) at initial diagnosis, and less than 20% of bladder cancers are muscle-invasive bladder cancers (MIBC). Low-grade (LG) NMIBC may arise from simple hyperplasia, and it is frequently characterized by FGFR3 mutation10. On the other hand, high-grade (HG) bladder cancer, thought to arise via flat dysplasia or carcinoma in situ, commonly has TP53 mutations11. The molecular features of LG NMIBC and MIBC are so distinct, that a “two-pathway model” has been proposed for bladder carcinogenesis12. Despite the differences in the molecular features between LG NMIBC and HG bladder cancer, most studies have focused primarily on MIBC using radical cystectomy samples. This is partly attributable to the ease of obtaining surgical specimens8,13. Li et al. investigated the landscape of somatic mutations in the morphologically normal urothelium of patients who underwent radical surgical removal; however, little is known about the mutational landscape of the normal urothelium of patients with LG NMIBC8.
TERT promoter mutation is one of the most frequent mutations in bladder cancer14. We previously reported that, in the non-malignant urothelium of patients with NMIBC, TERT promoter mutation is significantly associated with bladder tumor recurrence15 and is associated with the tumorigenesis of NMIBC16. However, the genomic evolution of the precancerous urothelium of LG NMIBC remains unclear. In this study, we aimed to investigate somatic mutations in the tumor and normal urothelium of patients with LG or HG NMIBC and analyze the genomic evolution of NMIBC.
Methods
Clinical samples
We randomly selected patients with NMIBC, who underwent transurethral resection of bladder tumor (TURBT) and systematic bladder biopsy at Osaka University Hospital and Kindai University Hospital and provided written informed consent. The study was approved by the Institutional Review Boards of Osaka University (IRB #668-3) and Kindai University (IRB #R02-155), and it conformed to the Declaration of Helsinki. Pathologically normal urothelium was obtained from systematic random biopsy performed at the time of TURBT. The diameter of the biopsy samples obtained by rigid biopsy forceps were about 4 mm, and we used all pathologically normal urothelium of random biopsy as a mixture for sequencing analysis. Tumor samples (pTa, pTis, or pT1), obtained via transurethral resection, were used.
Pathological diagnosis
The histological diagnoses were determined by at least two experienced pathologists. Tumor stage and grade were determined according to the American Joint Committee on Cancer (AJCC), 8th Edition Cancer Staging Manual17, and the tumors were graded according to the World Health Organization 2016 criteria18. For the analysis of normal urothelium we used only systematic biopsy samples diagnosed as non-malignant by the pathologist.
DNA extraction
DNA extraction from clinical specimens was performed using a GeneRead DNA FFPE Kit (QIAGEN, Hilden, Germany), as previously reported. DNA concentrations were measured using a Qubit dsDNA High-Sensitivity Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA). The purity of the extracted DNA was measured using Biospecnano (Shimadzu, Biotech, Japan).
Droplet digital polymerase chain reaction (ddPCR)
For mutation detection, the QX100 Droplet Digital PCR System (Bio-Rad Laboratories, Hercules, CA, USA), primers and probes (FAM, mutant type and HEX, wild type), and ddPCR Supermix for Probes (No dUTP), from Bio-Rad Laboratories, were used, as previously reported19.
Targeted sequence
A targeted DNA library, comprising 50 oncogenes and tumor suppressor genes for panel sequencing, was constructed using the Ion AmpliSeq Cancer Hotspot Panel v2 (Thermo Fisher Scientific), in accordance with the manufacturer’s recommended protocol. Briefly, 10 ng of DNA was subjected to multiplex PCR amplification using an Ion AmpliSeq Library Kit 2.0 and Ion AmpliSeq Cancer Hotspot Panel (Thermo Fisher Scientific), covering 50 genes. After multiplex PCR, Ion Xpress Barcode Adapters (Thermo Fisher Scientific) were ligated to the PCR products, which were then purified using Agencourt AMPure XP beads (Beckman Coulter, Brea, CA, USA)20. The purified libraries were pooled and sequenced using an Ion Torrent S5 instrument and Ion 550 Chip Kit (Thermo Fisher Scientific)21. DNA sequencing data were accessed using Torrent Suite ver. 5.12 program (Thermo Fisher Scientific)20. Reads were aligned against the hg19 human reference genome, and variants were called using the Variant Caller ver. 5.1221. The sequence quality of the samples was assessed by the on-target rate for hg19 and the total number of reads. Samples with mean depth < 500, and an on-target rate < 0.5, were excluded from further analysis. Raw variant calls were filtered by quality score < 50; depth of coverage < 20; synonymous variants; and manually checked using the integrative genomics viewer (IGV; Broad Institute, Cambridge, MA, USA). Germline mutations were excluded using the Human Genetic Variation Database (http://www.genome.med.kyoto-u.ac.jp/SnpDB) and Exome Aggregation Consortium database.
Detection of somatic mutations in normal urothelium using bioinformatics analysis
For the selection of biologically significant driver gene mutation in normal urothelium, the following inclusion criteria were used: (1) somatic mutations with variant allele frequency (VAF) > 0.1 in tumor specimen: or (2) manual review of aligned reads for confirmation with IGV. We reviewed manually with IGV for normal samples which we could not obtain the paired tumor specimens.
Results
Landscape of somatic mutation of tumor and normal urothelium of bladder
Twenty-seven tumors and 18 normal specimens from 22 patients with NMIBC were included in the analysis. Of these samples, 13 pairs of tumors and normal urothelium samples were obtained at the same TURBT from each patient. Patient characteristics are shown in Table 1. Of the 27 tumor specimens, 13 (48%) were pTa, 14 (52%) were pT1, and seven (26%) were diagnosed as concurrent carcinoma in situ (CIS). Twenty-four tumors were diagnosed as HG NMIBC, and 3 tumors were diagnosed as LG NMIBC. Of the 18 pathologically normal specimens, 4 (22%) were collected from patients with concurrent CIS. On average, we obtained a 29,911-fold coverage depth for the target regions in each specimen). The landscape of somatic mutations and variant allele frequency in the tumor and normal urothelium are shown in Fig. 1. Of the 27 tumor specimens, 25 (93%) had at least one somatic mutation. In contrast, 12 patients (67%) had at least one somatic mutation in the normal urothelium. Somatic mutations in TERT promoter regions, were most frequently identified in both tumor (44%) and normal samples (61%). FGFR3 mutation was also identified among LG, HG NMIBC and normal urothelium; but TP53 and PIK3CA mutations were detected only in tumor samples. CDKN2A mutation was identified in HG NMIBC and normal urothelium, but not in LG NMIBC. Because somatic mutation of TERT promoter and FGFR3, which were identified in the normal urothelium, have been reported as frequent mutations in tumor tissues by The Cancer Genome Atlas (TCGA), these mutations were thought to be potential drivers in the tumor formation of LG or HG NMIBC. There was no association between genomic alterations in the normal urothelium or tumors and the prognosis of patients with NMIBC.
Somatic mutation landscape of tumor and normal samples from patients with NMIBC. Clinical information and clinical samples used in this study (top), and the type of mutation and variant allele frequency (bottom) were shown in this landscape. The proportion mutations in both tumor and normal specimens were shown in left.
Paired analysis of somatic mutations in tumor and normal urothelium
Since some consistency is expected between the tumor and normal urothelium in the genomic evolution of bladder cancer, we performed paired analysis of the tumors and normal urothelium of patients with NMIBC obtained at the same time point (Fig. 2). As expected, somatic mutations in TERT promoter, FGFR3, and CDKN2A identified in the normal urothelium were consistently detected in tumor specimens in many cases. These data suggest that somatic mutations, such as in TERT promoter, FGFR3, or CDKN2A mutations, occur in cancer-initiated cells, and they may function as trunk events in the clonal expansion of NMIBC.
Comparison in somatic mutations in normal urothelium of patients with MIBC and those with LG or HG NMIBC
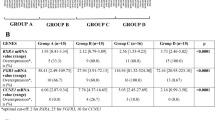
Because it is widely recognized that there is a huge difference in the genetic landscapes of LG NMIBC and MIBC, we focused on the difference in invasiveness of tumor specimens to further investigate the occurrence of putative driver mutations in the normal urothelium. Using previously published data on MIBC8 reported by Li et al., we compared the frequency of somatic mutations identified in both tumor and normal urothelium in Fig. 3A (LG and HG NMIBC) and Fig. 3B (MIBC). Careful interpretation is required because there are some differences regarding the ethnicity of patients, genomic sequencing methods, our small sample size and lack of data on TERT promoter mutations between the two cohorts. Somatic mutations identified in the normal urothelium of patients with MIBC are characterized by TP53 mutations, but not FGFR3 mutation. Genomic analysis of tumor and normal urothelium showed significant differences between MIBC and LG or HG NMIBC, and these differences could support the two-pathway model in bladder tumorigenesis. Finally, we investigated whether age could influence on the mutation frequency in NMIBC and MIBC (Table 2). The rate of TERT promoter mutations and TP53 in tumor specimens of patients with NMIBC were 4/13 (31%) and 7/13 (54%) in older age groups (stratified by median age), and 8/14 (57%) and 2/14 (14%) in younger age groups, but we could not observe these differences in normal urothelium. On the other hand, the rate of TP53 mutation in normal urothelium of patients with MIBC were 4/29 (14%) in older age groups, and 1/27 (4%) in younger age groups. The difference between age group might be associated with age-related mutation. Larger studies are needed to confirm these results.
Mutation frequency detected in tumor and normal urothelium. Mutation frequency of tumor samples (blue or light blue), and normal urothelium (orange) were shown. (A) Samples from patients with low-grade and high-grade non-muscle invasive bladder cancer. (B) Sample from patients with high-grade muscle invasive bladder cancer.
Discussion
Bladder cancer is thought to evolve from precancerous lesions, where cancer-initiating cells with pathologically normal appearances exist owing to field change. Several studies have identified distinct genomic features between LG and HG bladder cancer. LG NMIBC is characterized by gain-of-function mutations affecting oncogenes, such as FGFR3, HRAS, and PIK3CA, and deletions of chromosome 9q22,23,24. On the other hand, high-grade MIBC or metastatic bladder cancer, including carcinoma in situ, is characterized by loss-of-function mutations affecting tumor suppressor genes, such as TP53, RB, or PTEN25. Two separate genetic pathway models of bladder tumor progression have been proposed based on these differences12. For a deeper understanding of these two pathways in bladder tumorigenesis, it is important to perform molecular analysis of the normal urothelium of patients with bladder cancer. Li et al. investigated somatic clonal events in the normal urothelium of patients who underwent radical cystectomy for invasive bladder cancer, but little is known about somatic mutations in the normal urothelium of patients with LG or HG NMIBC, or about their difference between LG NMIBC and MIBC. In this study, we reported that TERT promoter, and FGFR3 somatic mutations characteristically recognized in the normal urothelium in LG or HG NMIBC could play important roles in tumorigenesis. We also showed that TP53 mutations are characteristically detected in the normal urothelium of MIBC but not in that of NMIBC. These observations were consistent with the genomic evolution model proposed by several researchers analyzing tumor specimens, supporting the two-tumorigenesis-pathway hypothesis of LG NMIBC and HG bladder cancer.
TERT promoter mutations are frequently detected in malignant tumors originating from normal cells with low rates of self-renewal26 such as glioblastoma26, melanoma27, and bladder cancer14,15. In bladder cancer, TERT promoter mutations occur in both precancerous lesions (27–63%)15,28 and high-grade tumors, including rare variant pathologies (57–100%) with aggressive phenotypes29,30,31,32,33. Cells with this mutation acquire the ability to escape cellular senescence by overcoming replicative immortality, leading to genomic instability and tumorigenesis34. The frequency of TERT promoter mutation in NMIBC was higher in normal urothelium than that in tumor in current study, these data could possibly indicate that tumorigenesis of NMIBC was associated with TERT promoter mutation. Somatic mutations in FGFR3 are more frequently detected in NMIBC (39%)35 than in MIBC (14%)36. FGFR3 mutations occur in urothelial hyperplasia of the bladder and are thought to be associated with tumor formation in NMIBC10. CDKN2A tumor suppressor genes play crucial roles in the cell cycle and in senescence37. Several researchers have reported that genetic and epigenetic alterations in CDKN2A lead to tumorigenesis and poor prognosis in patients with malignant tumor37,38. TP53 mutations are frequently detected in various types of cancer39. These mutations are rarely detected in low-grade bladder cancer35, but are frequently detected in high-grade bladder cancer, including carcinoma in situ36. This may indicate that TP53 mutations are early events in tumorigenesis, in high-grade bladder tumors or carcinomas in situ.
Several researchers reported that mutant DNA could be detected in the urine of patients with no evidence of cancer, and it was associated with subsequent bladder cancer development19,40,41. In our previous report41 about patients under surveillance after TURBT for NMIBC, patients with TERT C228T mutation in urinary cell-free DNA after TURBT experienced significantly higher bladder recurrence rate than those without TERT C228T mutation in urine collected after TURBT. Though there was a possibility that the bladder tumor was too small to be detected by cystoscopy, our current study suggests that mutant DNA present in the normal urothelium during the early stages of tumor formation may be released into the urine. Furthermore, genomic analysis of normal urothelium using urine samples can reflect the comprehensive molecular status of the normal urothelium and may be used to predict bladder cancer development or recurrence of NMIBC.
This study had several limitations. First, it was a retrospective pilot study with a small sample size. Owing to the small sample size, it was difficult to examine the association between mutation patterns in the normal urothelium and prognosis in bladder cancer, and analyze the genomic difference of normal urothelium between NMIBC and MIBC statistically in the current study. Second, our study lacked a comprehensive dataset for genomic analysis. We examined the normal urothelium of Japanese patients with NMIBC using 50-gene targeted panel. In contrast, we used public data available for the analysis of the normal urothelium in patients with MIBC.
Further comprehensive genomic analyses of the normal urothelium of patients with both NMIBC and MIBC could provide a deeper understanding of the role of somatic mutations in bladder tumorigenesis.
Conclusions
Our data indicated that LG, HG NMIBC and MIBC have distinct features of precancerous lesions by comprehensively analyzing the normal urothelium of bladder tumors. The identification of this difference between NMIBC and MIBC may improve the current understanding of bladder tumor development, paving the way for better treatment strategies.
Data availability
The datasets generated during and/or analyzed during the current study are available in the SRA repository, [http://www.ncbi.nlm.nih.gov/bioproject/845018].
Abbreviations
- CDKN2A:
-
Cyclin dependent kinase inhibitor 2A
- FGFR3:
-
Fibroblast growth factor receptor 3
- HRAS:
-
Harvey rat sarcoma
- PIK3CA:
-
Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha
- PTEN:
-
Phosphatase and tensin homolog deleted from chromosome 10
- TERT:
-
Telomerase reverse transcriptase
- TP53:
-
Tumor protein p53
- NMIBC:
-
Non-muscle invasive bladder cancer
- MIBC:
-
Muscle invasive bladder cancer
- RB:
-
Retinoblastoma
References
Fearon, E. R. & Vogelstein, B. A genetic model for colorectal tumorigenesis. Cell 61, 759–767 (1990).
Lee-Six, H. et al. The landscape of somatic mutation in normal colorectal epithelial cells. Nature 574, 532–537 (2019).
Brunner, S. F. et al. Somatic mutations and clonal dynamics in healthy and cirrhotic human liver. Nature 574, 538–542 (2019).
Martincorena, I. et al. Somatic mutant clones colonize the human esophagus with age. Science 362, 911–917 (2018).
Martincorena, I. et al. Tumor evolution. High burden and pervasive positive selection of somatic mutations in normal human skin. Science 348, 880–6 (2015).
Yoshida, K. et al. Tobacco smoking and somatic mutations in human bronchial epithelium. Nature 578, 266–272 (2020).
Lee-Six, H. et al. Population dynamics of normal human blood inferred from somatic mutations. Nature 561, 473–478 (2018).
Li, R. et al. Macroscopic somatic clonal expansion in morphologically normal human urothelium. Science 370, 82–89 (2020).
Lawson, A. R. J. et al. Extensive heterogeneity in somatic mutation and selection in the human bladder. Science 370, 75–82 (2020).
van Oers, J. M. et al. Chromosome 9 deletions are more frequent than FGFR3 mutations in flat urothelial hyperplasias of the bladder. Int. J Cancer 119, 1212–1215 (2006).
Hartmann, A. et al. Occurrence of chromosome 9 and p53 alterations in multifocal dysplasia and carcinoma in situ of human urinary bladder. Cancer Res. 62, 809–818 (2002).
Knowles, M. A. & Hurst, C. D. Molecular biology of bladder cancer: New insights into pathogenesis and clinical diversity. Nat. Rev. Cancer 15, 25–41 (2015).
Majewski, T. et al. Whole-organ genomic characterization of mucosal field effects initiating bladder carcinogenesis. Cell Rep. 26, 2241–2256 (2019).
Borah, S. et al. Cancer. TERT promoter mutations and telomerase reactivation in urothelial cancer. Science 347, 1006–10 (2015).
Hayashi, Y. et al. TERT C228T mutation in non-malignant bladder urothelium is associated with intravesical recurrence for patients with non-muscle invasive bladder cancer. Mol. Oncol. 14, 2375–2383 (2020).
Hayashi, Y. et al. Telomerase reverse transcriptase promoter mutation in tumorigenesis of bladder cancer: Evolutionary trajectory by algorithmic inference from cross-sectional data. Int. J. Urol. 28, 774–776 (2021).
Amin, M. B. et al. AJCC Cancer Staging Manual, eighth ed. (2017).
Moch, H., Humphrey, P. A., Ulbright, T. M.& Reuter, V. E. International Agency for Research on Cancer: WHO Classification of Tumours of Urinary System and Male Genital Organs, fourth ed. (2016).
Hayashi, Y. et al. Diagnostic potential of TERT promoter and FGFR3 mutations in urinary cell-free DNA in upper tract urothelial carcinoma. Cancer Sci. 110, 1771–1779 (2019).
Sakai, K. et al. Clonal composition of human ovarian cancer based on copy number analysis reveals a reciprocal relation with oncogenic mutation status. Cancer Lett. 405, 22–28 (2017).
Noguchi, T. et al. Comprehensive gene mutation profiling of circulating tumor DNA in ovarian cancer: Its pathological and prognostic impact. Cancers (Basel) 12, 3382 (2020).
Ploussard, G. et al. Prognostic value of loss of heterozygosity at chromosome 9p in non-muscle-invasive bladder cancer. Urology 76, 513 (2010).
Krüger, S., Mahnken, A., Kausch, I. & Feller, A. C. P16 immunoreactivity is an independent predictor of tumor progression in minimally invasive urothelial bladder carcinoma. Eur. Urol. 47, 463–467 (2005).
Bartoletti, R. et al. Loss of P16 expression and chromosome 9p21 LOH in predicting outcome of patients affected by superficial bladder cancer. J. Surg. Res. 143, 422–427 (2007).
Castillo-Martin, M., Domingo-Domenech, J., Karni-Schmidt, O., Matos, T. & Cordon-Cardo, C. Molecular pathways of urothelial development and bladder tumorigenesis. Urol. Oncol. 28, 401–408 (2010).
Killela, P. J. et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc. Natl. Acad. Sci. U. S. A. 110, 6021–6 (2013).
Huang, F. W. et al. Highly recurrent TERT promoter mutations in human melanoma. Science 339, 957–959 (2013).
Rodriguez, P. M. D. C. et al. Spectrum of genetic mutations in de novo PUNLMP of the urinary bladder. Virchows Arch. 471, 761–767 (2017).
Nguyen, D. et al. High prevalence of TERT promoter mutations in micropapillary urothelial carcinoma. Virchows Arch. 469, 427–434 (2016).
Cowan, M. L. et al. Detection of TERT promoter mutations in primary adenocarcinoma of the urinary bladder. Hum. Pathol. 53, 8–13 (2016).
Cowan, M. et al. High prevalence of TERT promoter mutations in primary squamous cell carcinoma of the urinary bladder. Mod. Pathol. 29, 511–515 (2016).
Zheng, X. et al. High frequency of TERT promoter mutation in small cell carcinoma of bladder, but not in small cell carcinoma of other origins. J. Hematol. Oncol. 7, 47. https://doi.org/10.1186/s13045-014-0047-7 (2014).
Palsgrove, D. N. et al. Targeted sequencing of plasmacytoid urothelial carcinoma reveals frequent TERT promoter mutations. Hum. Pathol. 85, 1–9 (2019).
Chiba, K. et al. Mutations in the promoter of the telomerase gene TERT contribute to tumorigenesis by a two-step mechanism. Science 357, 1416–1420 (2017).
Pietzak, E. J. et al. Next-generation sequencing of nonmuscle invasive bladder cancer reveals potential biomarkers and rational therapeutic targets. Eur. Urol. 72, 952–959 (2017).
Robertson, A. G. et al. Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 174, 1033 (2018).
Nabel, E. G. CDKs and CKIs: Molecular targets for tissue remodelling. Nat. Rev. Drug Discov. 1, 587–598 (2002).
Witcher, M. & Emerson, B. M. Epigenetic silencing of the p16(INK4a) tumor suppressor is associated with loss of CTCF binding and a chromatin boundary. Mol. Cell. 34, 271–284 (2009).
Petitjean, A., Achatz, M. I., Borresen-Dale, A. L., Hainaut, P. & Olivier, M. TP53 mutations in human cancers: Functional selection and impact on cancer prognosis and outcomes. Oncogene 26, 2157–2165 (2007).
Springer, S. U. et al. Non-invasive detection of urothelial cancer through the analysis of driver gene mutations and aneuploidy. Elife 7, e32143. https://doi.org/10.7554/eLife.32143 (2018).
Hayashi, Y. et al. Clinical significance of hotspot mutation analysis of urinary cell-free DNA in urothelial bladder cancer. Front. Oncol. 10, 755. https://doi.org/10.3389/fonc.2020.00755 (2020).
Acknowledgements
We thank all other researchers in our laboratory.
Funding
This study was supported by JSPS KAKENHI Grant Number JP 20K18139, Kobayashi Foundation for Cancer Research and Young Research Grant from The Japanese Urological Association.
Author information
Authors and Affiliations
Contributions
H.: Conceptualization, formal analysis, methodology, investigation, writing-original draft. K.F.: Conceptualization, supervision, writing-review and editing. K.S: Sequence analysis. S.A.: Investigation, sample collection. E.B.: Supervision, sample collection. S.N.: Pathological diagnosis. E.T.: Supervision, sample collection. M.M.: Supervision, sample collection. T.K.: Supervision. K.H.: Supervision. A.K.: Supervision. T.M.: Supervision, Sample collection. E.M.: Pathological diagnosis. H.U.: Supervision. K.N.: Sequence analysis. N.N.: Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hayashi, Y., Fujita, K., Sakai, K. et al. Targeted-sequence of normal urothelium and tumor of patients with non-muscle invasive bladder cancer. Sci Rep 12, 16642 (2022). https://doi.org/10.1038/s41598-022-21158-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21158-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.