Abstract
We aimed to evaluate the association between ICU patient volume before the COVID-19 pandemic and the outcomes of ventilated COVID-19 patients. We analyzed ventilated patients with COVID-19 aged > 17 years and enrolled in the J-RECOVER study, a retrospective multicenter observational study conducted in Japan between January and September 2020. Based on the number of patients admitted to the ICU between January and December 2019, the top third institutions were defined as high-volume centers, the middle third ones as middle-volume centers, and the bottom third ones as low-volume centers. The primary outcome measure was in-hospital mortality. Multivariate logistic regression analysis for in-hospital mortality and ICU patient volume was performed after adjusting for multiple propensity scores. Among 461 patients, 158, 158, and 145 patients were admitted to low-volume (20 institutions), middle-volume (14 institutions), and high-volume (13 institutions) centers, respectively. Admission to middle- and high-volume centers was not significantly associated with in-hospital death compared with admission to low-volume centers (adjusted odds ratio, 1.11 [95% confidence interval (CI): 0.55–2.25] and adjusted odds ratio, 0.81 [95% CI: 0.31–1.94], respectively). In conclusion, institutional intensive care patient volume prior to the COVID-19 pandemic was not significantly associated with in-hospital death in ventilated COVID-19 patients.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has become a major burden on health care systems worldwide1. One-fifth to one-third of hospitalized patients with COVID-19 become critically ill, and two-thirds of critically ill patients require invasive mechanical ventilation2,3,4,5. The case-fatality rate for these patients on mechanical ventilation has been reported to be approximately 45%6. The COVID-19 pandemic has resulted in an extreme increase in demand for intensive care unit (ICU) resources. Improvements in the health care system and survival rates for severe COVID-19 are urgent issues.
An increase in the number of medical and surgical patients improves the prognosis of patients, especially those who are critically ill or have undergone complex surgical procedures7,8. Many studies suggest that ICU patient outcomes are related to the number of patients treated and the number of beds available8,9,10,11,12,13,14. Therefore, critically ill patients may be best treated in the ICU, where more high-risk patients are treated. However, there are also reports that the volume-outcome relationship was not observed15,16,17,18,19 and that patient outcomes are worse in hospitals with a high number of ventilated patients or high ICU occupancy rate20,21. Few studies have examined whether the outcome of COVID-19 ICU patients is better in hospitals that are accustomed to treating a high volume of ICU patients. The examination of the volume-outcome relationship in terms of the usual number of ICU patients and severe COVID-19 may help improve the care, outcomes, and health care system of COVID-19 ICU patients.
We hypothesized that routine treatment of a large number of ICU patients and proficiency in ICU care would be associated with better outcomes in COVID-19 ICU patients. To evaluate our hypothesis, we investigated the association between institutional ICU patient volume before the COVID-19 pandemic and outcomes in ventilated ICU COVID-19 patients.
Methods
Study design and setting
The current study was one of the data analyses from the J-RECOVER study. The J-RECOVER study was a retrospective multicenter observational study conducted in Japan between January and September 2020. The design, data collection methods, and protocols of the J-RECOVER study have been previously reported in detail22. The current study was performed in accordance with the Declaration of Helsinki. The present study was approved by the institutional review boards of Nippon Medical School Musashikosugi Hospital (representative institution, application number:561-2-26), and the requirement for informed consent was waived because of the anonymous nature of the data used. Treatment protocols were left to each institution.
Patients
The J-RECOVER study included COVID-19 patients admitted to the participating institutions during the study period. The present study included ventilated patients with severe COVID-19 aged > 17 years and were enrolled in the J-RECOVER study. Patients were excluded if they had missing data on the number of ICU admissions in 2019 at the institution.
Data collection
The patients’ clinical information was obtained from diagnosis procedure combination (DPC) data and medical records. The DPC system is comprehensively evaluated for acute inpatient care costs. Administrative billing data have been created and stored electronically at each institution under a comprehensive payment system based on DPC22,23. DPC data included sex, date of birth, the primary purpose of care during hospitalization, date of admission, date of discharge, transportation of the patient, route of admission, hospital referral or outpatient department admission, scheduled or emergency care admission, emergency ambulance transport, discharge destination, and the outcomes of discharge. In addition, other necessary information that was not available from the DPC data was obtained from the institutions’ medical records and personnel.
Measurements and definitions
The primary outcome measure was in-hospital death due to COVID-19 during hospitalization. Intensive care volume was defined as the number of patients admitted to the ICU between January and December 2019, the year before the COVID-19 pandemic, and it was subdivided into three categories, as per previous studies12,24,25 to evaluate the dose–response relationship. A cutoff number was defined to determine the number of patients as evenly as possible. The top third institutions were defined as high-volume centers, the middle third ones as middle-volume centers, and the bottom third ones as low-volume centers. We used the Charlson comorbidity index to measure underlying disease26. We used the Sequential Organ Failure Assessment (SOFA) score as an index of severity27.
Statistical analysis
Demographic factors, patient characteristics, hospital care, and outcomes were compared among patients treated in high-, middle-, and low-volume centers. We analyzed trends in discrete variables among the three groups using the Mantel–Haenszel trend test and analyzed continuous variables using the Kruskal–Wallis test.
Regarding missing values, we performed multiple imputations28. Twenty multiple imputed datasets were generated. We performed multivariate logistic regression analyses to evaluate the association between ICU case volume and in-hospital death in each dataset, and the estimates were then combined.
Multiple propensity score analysis was used in the multivariate analysis to adjust for measurable prehospital confounding factors29,30. The propensity score indicates the conditional probability of a specific exposure given a series of measured baseline variables and is a well-established method for reducing confounding effects in observational studies. The propensity score is used to compare two groups; however, the multiple propensity score was used since this was a comparison of three groups30,31,32. Moreover, instead of matching and IPTW, which are frequently used in the comparison of two groups using propensity scores, multiple propensity scores were used as covariates in the multivariate analysis to adjust for confounding factors since this is a three-group comparison. A multiple propensity score is the conditional probability of being classified into three or more specific groups, given a set of observed baseline covariates. We adapted a multinomial logistic regression model to estimate the multiple propensity score for the present analysis. The model fell into one of the three groups along with hospital characteristics, including teaching status, number of hospital beds, number of ICU beds, patient demographics (age, sex, and Charlson comorbidity index), and prehospital factors (number of days from symptom onset to hospitalization, number of days from positive polymerase chain reaction test to hospitalization, transfer from another hospital, and SOFA score). Multivariate logistic regression was then used to analyze the association between ICU volume and in-hospital mortality, adjusting for multiple propensity scores and in-hospital variables such as favipiravir, remdesivir, ICU admission, use of prone position, and use of extracorporeal membrane oxygenation (ECMO), while also adjusting for within-hospital clustering using a generalized estimating equation.
All statistical analyses were two-sided, and a level of 0.05 was considered statistically significant. We analyzed the data using SPSS statistical software version 26 (IBM, New York, USA).
Results
Patients
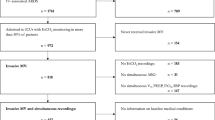
The J-RECOVER study enrolled 4,700 patients with COVID-19 from 66 institutions. Among them, 561 patients aged > 17 years required ventilator management (Fig. 1). After excluding 100 cases with missing data on the number of ICU admissions in 2019 at the institution where they were admitted, 461 patients were included in the analyses. A total of 158, 158, and 145 patients were admitted to low-volume (20 institutions), middle-volume (14 institutions), and high-volume (13 institutions) centers, respectively. There were no ventilated patients in 11 institutions, and there were no data on the number of ICU admissions in 2019 in 8 institutions that had ventilated patient admissions.
Institutional information and patient characteristics
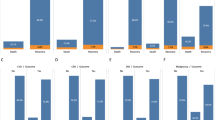
There were no significant differences in the number of academic hospitals, hospital beds, patients per institution, and ECMO patients per institution among the three groups (Table 1). Higher ICU case volume showed a significant tendency of higher ICU beds (< 0.001).
Characteristics of the study population were described in Table 2. The proportion of men in the high-volume center was significantly higher than that of men in the other two groups (p = 0.04). Higher ICU case volume showed a significantly lower SOFA score on admission (p = 0.03). Patients in middle-volume centers had a lower probability of prone position (p < 0.001).
The differences in outcomes among institutions
There were no significant differences in transfer to another department, transfer to another hospital, length of stay in the hospital, length of stay in ICU, and in-hospital death among the three groups (Table 3).
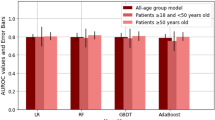
Multivariate logistic regression analyses for 1 month survival adjusted by multiple propensity score
Admission to middle-volume centers was not significantly associated with in-hospital mortality compared with admission to low-volume centers (adjusted odds ratio, 1.11 [95% confidence interval (CI): 0.55–2.25]. In addition, high-volume centers were not significantly associated with in-hospital mortality compared to admission to low-volume centers (adjusted odds ratio, 0.81 95% CI: 0.31–1.94) after adjustment for multiple propensity scores and in-hospital variables (Table 4).
Discussion
The current study evaluated the association between the institutional ICU patient volume before the COVID-19 pandemic and in-hospital mortality in ventilated COVID-19 patients. There was no significant association between the institutional ICU case volume in 2019 and in-hospital death after adjusting for patient characteristics, institutional information, and prehospital and in-hospital confounding factors. Since there was minimal bias in the proportion of academic hospitals, staffing ratio, advanced treatments such as ECMO, prone ventilation among the groups, size effect of result, and no dose–response relationship of volume-outcome, low-volume center may not worsen the outcome for severe COVID-19. The findings from the present study may be useful in developing a medical system for patients with severe COVID-19.
While many previous studies evaluated the volume-outcome relationships in critical care and found that high patient volumes may improve survival outcomes8,9,10,11,12,13,14, several studies found no association15,16,17,18,19. Some studies observed that high patient volumes may be associated with worse outcomes20,21. These variances among study findings may be due to differences in health care systems and hospital types, ICU management developments, or differences in statistical methods. What differentiated this study from previous volume-outcome relationship studies regarding the number of ICU patients treated and their outcomes is that it examined the association between the number of pre-pandemic ICU patients and the outcomes of COVID-19 ICU patients. In other words, our study examined whether institutions accustomed to ICU care can improve the outcomes of COVID-19 ICU patients. We hypothesized that severely ill COVID-19 patients would be best treated in ICUs that have treated higher-risk patients. However, contrary to our hypothesis, our study did not observe a significant association between the institutional ICU patient volume before the COVID-19 pandemic and in-hospital mortality.
Several reasons could explain why there was no significant association between institutional ICU patient volume and outcomes for COVID-19 ventilated cases. Many of the participating hospitals in this study were tertiary emergency centers. Both centers with high and low ICU patient volume in 2019 may have been habitually proficient in ICU care. There was minimal bias among the groups in staffing ratios of emergency medicine and intensive care specialists. In addition, the Ministry of Health, Labour and Welfare (MHLW) has set a standard of (at least) one nurse per two patients in all ICU. Advanced treatments such as ECMO and prone positioning were equally or more frequently performed at the smaller institutions. The availability of staff resources, even in smaller institutions, may be one of the factors that contributed to the absence of a volume-outcome relationship. The number of COVID-19 patients during the study period was also less biased among the three groups, suggesting that the ICU burden from COVID-19 was not unbalanced. In addition, ICU resources for severe COVID-19 were maintained in Japan during the study period33. In an ICU such as that in Japan, that is, a system in which there are more than a certain number of emergency physicians, intensivists, and nurses at the facility for each patient, there may not be a volume-outcome relationship. Further large-scale study is needed to evaluate this generated hypothesis.
Previous studies examining volume-outcome relationships for ICU care have included patients with varying diseases rather than patients with a specific disease or intervention34. The overall impact is therefore unclear. The study included COVID-19 patients who were on ventilator management, giving a relatively clear depiction of the patient population. Multiple propensity scores were also used to adjust for many confounding factors such as patient characteristics, institutional information, and prehospital and in-hospital factors. Few studies have examined the association between ICU patient volume prior to the COVID-19 pandemic and the outcomes of COVID-19 ICU patients. These results are considered important for constructing a health care system.
There were several limitations in the present study. First, this study did not have a large number of eligible institutions and cases. Thus, although this study did not find a significant difference between ICU patient volume and outcome, a volume-outcome relationship could not be ruled out. Further prospective large-scale studies are needed to assess the association between ICU patient volume and the outcomes of patients with severe COVID-19. Second, the J-RECOVER study was not a population-based study and was conducted at a volunteer hospital. The generalization of the results may be limited. Third, several patients were excluded due to missing ICU admission data in 2019. Since the data are per-institution, patients were missing on a per-institution basis, and the impact on the results is unknown.
Conclusions
In the present study, institutional ICU patient volume prior to the COVID-19 pandemic was not significantly associated with in-hospital death in ventilated COVID-19 patients after adjusting for patient demographics, institutional information, and prehospital and in-hospital factors. In ICUs with adequate staff resources, small institution may not worsen the outcome. Further prospective large-scale study is needed to determine the association between institutional ICU patient volumes and severe COVID-19 outcomes.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available because the use of the data was limited to institutions that participated in the registry. Datasets are available from the corresponding author upon reasonable request.
References
Remuzzi, A. & Remuzzi, G. COVID-19 and Italy: What next?. Lancet 395, 1225–1228 (2020).
Abate, S. M., Ahmed Ali, S., Mantfardo, B. & Basu, B. Rate of intensive care unit admission and outcomes among patients with coronavirus: A systematic review and meta-analysis. PLoS ONE 15, e0235653 (2020).
Docherty, A. B. et al. Features of 20133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ 369, m1985 (2020).
Cummings, M. J. et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 395, 1763–1770 (2020).
Tan, E., Song, J., Deane, A. M. & Plummer, M. P. Global impact of coronavirus disease 2019 infection requiring admission to the ICU: A systematic review and meta-analysis. Chest 159, 524–536 (2021).
Lim, Z. J. et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation. A meta-analysis. Am. J. Respir. Crit. Care Med. 203, 54–66 (2021).
Halm, E. A., Lee, C. & Chassin, M. R. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann. Intern. Med. 137, 511–520 (2002).
Nguyen, Y. L. et al. The volume-outcome relationship in critical care: A systematic review and meta-analysis. Chest 148, 79–92 (2015).
Kahn, J. M. et al. Hospital volume and the outcomes of mechanical ventilation. N. Engl. J. Med. 355, 41–50 (2006).
Needham, D. M. et al. Hospital volume and mortality for mechanical ventilation of medical and surgical patients: A population-based analysis using administrative data. Crit. Care Med. 34, 2349–2354 (2006).
Kahn, J. M., Ten Have, T. R. & Iwashyna, T. J. The relationship between hospital volume and mortality in mechanical ventilation: An instrumental variable analysis. Health Serv. Res. 44, 862–879 (2009).
Ike, J. D., Kempker, J. A., Kramer, M. R. & Martin, G. S. The association between acute respiratory distress syndrome hospital case volume and mortality in a U.S. cohort, 2002–2011. Crit. Care Med. 46, 764–773 (2018).
Glance, L. G., Li, Y., Osler, T. M., Dick, A. & Mukamel, D. B. Impact of patient volume on the mortality rate of adult intensive care unit patients. Crit. Care Med. 34, 1925–1934 (2006).
Kahn, J. M. et al. Potential value of regionalized intensive care for mechanically ventilated medical patients. Am. J. Respir. Crit. Care Med. 177, 285–291 (2008).
Fernández, R. et al. Relationship between volume and survival in closed intensive care units is weak and apparent only in mechanically ventilated patients. Anesthesiology 119, 871–879 (2013).
Cooke, C. R. et al. Despite variation in volume, Veterans Affairs hospitals show consistent outcomes among patients with non-postoperative mechanical ventilation. Crit. Care Med. 40, 2569–2575 (2012).
Gopal, S., O’Brien, R. & Pooni, J. The relationship between hospital volume and mortality following mechanical ventilation in the intensive care unit. Minerva Anestesiol. 77, 26–32 (2011).
Moran, J. L. & Solomon, P. J. ANZICS Centre for Outcome and Resource Evaluation of the Australian and New Zealand Intensive Care Society. Mortality and intensive care volume in ventilated patients from 1995 to 2009 in the Australian and New Zealand binational adult patient intensive care database. Crit. Care Med. 40, 800–812 (2012).
Durairaj, L. et al. Hospital volume-outcome relationships among medical admissions to ICUs. Chest 128, 1682–1689 (2005).
Mehta, A. B., Walkey, A. J., Curran-Everett, D., Matlock, D. & Douglas, I. S. Hospital mechanical ventilation volume and patient outcomes: Too much of a good thing?. Crit. Care Med. 47, 360–368 (2019).
Lapichino, G. et al. Volume of activity and occupancy rate in intensive care units. Association with mortality. Intensive Care Med. 30, 209–297 (2004).
Tagami, T. et al. Japanese multicenter research of COVID-19 by assembling real-world data: A study protocol. Ann. Clin. Epidemiol. 4, 92–100 (2022).
Yasunaga, H. Real world data in Japan: Chapter II The diagnosis procedure combination database. Ann. Clin. Epidemiol. 1, 76–79 (2019).
Sasabuchi, Y. et al. The volume-outcome relationship in critically ill patients in relation to the ICU-to-hospital bed ratio. Crit. Care Med. 43, 1239–1245 (2015).
Kluge, G. H. et al. The association between ICU level of care and mortality in the Netherlands. Intensive Care Med. 41, 304–311 (2015).
Quan, H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 43, 1130–1139 (2005).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710 (1996).
Sterne, J. A. et al. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 338, b2393 (2009).
Feng, P., Zhou, X. H., Zou, Q. M., Fan, M. Y. & Li, X. S. Generalized propensity score for estimating the average treatment effect of multiple treatments. Stat. Med. 31, 681–697 (2012).
Spreeuwenberg, M. D. et al. The multiple propensity score as control for bias in the comparison of more than two treatment arm: An introduction from a case study in mental health. Med. Care 48, 166–174 (2010).
Tagami, T., Matsui, H., Fushimi, K. & Yasunaga, H. Changes in therapeutic hypothermia and coronary intervention provision and in-hospital mortality of patients with out-of-hospital cardiac arrest: A nationwide database study. Crit. Care Med. 44, 488–495 (2016).
Amagasa, S. et al. Relationship between institutional case volume and one-month survival among cases of paediatric out-of-hospital cardiac arrest. Resuscitation 137, 161–167 (2019).
Japan ECMOnet for COVID-19, Shime, N. Save the ICU and save lives during the COVID-19 pandemic. J. Intensive Care 8, 40 (2020).
Dodek, P. Volume-outcome relationships in critical care. Understanding the mechanism. Am. J. Respir. Crit. Care Med. 190, 601–603 (2014).
Author information
Authors and Affiliations
Contributions
S.A. designed the study, analyzed the data, and drafted the manuscript. M.H., K.Y., A.E., T.O., A.H., H.Y., and T.T. designed the J-RECOVER database. T.T. coordinated and supervised the data collection. M.K., H.Y., and T.T. critically revised the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amagasa, S., Kashiura, M., Yasuda, H. et al. Relationship between institutional intensive care volume prior to the COVID-19 pandemic and in-hospital death in ventilated patients with severe COVID-19. Sci Rep 12, 22318 (2022). https://doi.org/10.1038/s41598-022-26893-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26893-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.