Abstract
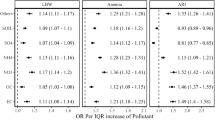
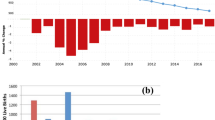
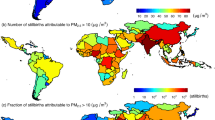
India has one of the highest (53%) global prevalences of anaemia among women of reproductive age (WRA, 15–49 years). Long-term exposure to ambient fine particulate matter (PM2.5), a type of air pollution, may increase the prevalence of anaemia through systemic inflammation. Using a linear mixed model adjusted for potential confounding factors, we show that for every 10 µg m−3 increase in ambient PM2.5 exposure, the average anaemia prevalence among Indian WRA increases by 7.23% (95% uncertainty interval, 6.82–7.63). Among PM2.5 species, sulfate and black carbon are more associated with anaemia than organics and dust. Among sectoral contributors, industry was the greatest, followed by the unorganized, domestic, power, road dust, agricultural waste burning and transport sectors. If India meets its recent clean-air targets, such anaemia prevalence among WRA will fall from 53% to 39.5%, taking 186 districts below the national target of 35%. Our results suggest that the transition to clean energy would accelerate India’s progress towards the ‘anaemia-free’ mission target.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The satellite-based PM2.5 data that support the findings of this study are available in the Code Ocean database (https://codeocean.com/capsule/5860976/tree). The MERRA-2 reanalysis data were retrieved from https://gmao.gsfc.nasa.gov/reanalysis/MERRA-2/. The model data used in this study are available from the corresponding author on reasonable request. DHS data source: https://www.dhsprogram.com/data/available-datasets.cfm.
Code availability
The code that supports the findings of this study is available in the Code Ocean database (https://codeocean.com/capsule/5860976/tree) and from the corresponding author on reasonable request.
References
Kassebaum, N. J. The global burden of anemia. Hematol. Oncol. Clin. North Am. 30, 247–308 (2016).
Kinyoki, D., Osgood-Zimmerman, A. E., Bhattacharjee, N. V., Kassebaum, N. J. & Hay, S. I. Anemia prevalence in women of reproductive age in low- and middle-income countries between 2000 and 2018. Nat. Med. 27, 1761–1782 (2021).
Global Nutrition Targets 2025: Policy Brief Series (WHO, 2014); https://www.who.int/publications-detail-redirect/WHO-NMH-NHD-14.2
Wirth, J. P. et al. Predictors of anemia in women of reproductive age: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am. J. Clin. Nutr. 106, 416S–427S (2017).
Swaminathan, S. et al. The burden of child and maternal malnutrition and trends in its indicators in the states of India: the Global Burden of Disease Study 1990–2017. Lancet Child Adolesc. Health 3, 855–870 (2019).
National Family Health Survey (NFHS-4), 2015–16 (IIPS and ICF, 2017); https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf
Kapil, U., Kapil, R. & Gupta, A. National iron plus initiative: current status & future strategy. Indian J. Med. Res. 150, 239–247 (2019).
Ghosh, S., Sinha, S., Thomas, T., Sachdev, H. S. & Kurpad, A. V. Revisiting dietary iron requirement and deficiency in Indian women: implications for food iron fortification and supplementation. J. Nutr. 149, 366–371 (2019).
Morales-Ancajima, V. C. et al. Increased outdoor PM2.5 concentration is associated with moderate/severe anemia in children aged 6–59 months in Lima, Peru. J. Environ. Public Health 2019, e6127845 (2019).
Stauder, R., Valent, P. & Theurl, I. Anemia at older age: etiologies, clinical implications, and management. Blood 131, 505–514 (2018).
Honda, T., Pun, V. C., Manjourides, J. & Suh, H. Anemia prevalence and hemoglobin levels are associated with long-term exposure to air pollution in an older population. Environ. Int. 101, 125–132 (2017).
Elbarbary, M. et al. Ambient air pollution exposure association with anaemia prevalence and haemoglobin levels in Chinese older adults. Int. J. Environ. Res. Public Health 17, 3209 (2020).
Cohen, A. J. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389, 1907–1918 (2017).
Dandona, L. et al. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet 390, 2437–2460 (2017).
Spears, D. et al. The association of early-life exposure to ambient PM2.5 and later-childhood height-for-age in India: an observational study. Environ. Health 18, 62 (2019).
Balakrishnan, K. et al. Exposures to fine particulate matter (PM2.5) and birthweight in a rural–urban, mother–child cohort in Tamil Nadu, India. Environ. Res. 161, 524–531 (2018).
Mehta, U. et al. The association between ambient PM2.5 exposure and anemia outcomes among children under five years of age in India. Environ. Epidemiol. 5, e125 (2021).
Ostro, B., Feng, W.-Y., Broadwin, R., Green, S. & Lipsett, M. The effects of components of fine particulate air pollution on mortality in California: results from CALFINE. Environ. Health Perspect. 115, 13–19 (2007).
Janssen, N. A. H. et al. Black carbon as an additional indicator of the adverse health effects of airborne particles compared with PM10 and PM2.5. Environ. Health Perspect. 119, 1691–1699 (2011).
Lippmann, M., Chen, L.-C., Gordon, T., Ito, K. & Thurston, G. D. National Particle Component Toxicity (NPACT) Initiative: integrated epidemiologic and toxicologic studies of the health effects of particulate matter components. Res. Rep. Health Eff. Inst. 177, 5–13 (2013).
Swaminathan, S. et al. Dietary iron intake and anemia are weakly associated, limiting effective iron fortification strategies in India. J. Nutr. 149, 831–839 (2019).
Dey, S. et al. A satellite-based high-resolution (1-km) ambient PM2.5 database for India over two decades (2000–2019): applications for air quality management. Remote Sens. 12, 3872 (2020).
Bali, K., Dey, S. & Ganguly, D. Diurnal patterns in ambient PM2.5 exposure over India using MERRA-2 reanalysis data. Atmos. Environ. 248, 118180 (2021).
Villalobos, A. M. et al. Source apportionment of carbonaceous fine particulate matter (PM2.5) in two contrasting cities across the Indo–Gangetic Plain. Atmos. Pollut. Res. 6, 398–405 (2015).
GBD MAPS Working Group. Burden of Disease Attributable to Major Air Pollution Sources in India (HEI, 2018).
Ganguly, T., Selvaraj, K. L. & Guttikunda, S. K. National Clean Air Programme (NCAP) for Indian cities: review and outlook of clean air action plans. Atmos. Environ.: X 8, 100096 (2020).
Ranjan, R. & Singh, S. Household cooking fuel patterns in rural India: pre- and post-Pradhan Mantri Ujjwala Yojana. Indian J. Hum. Dev. 14, 518–526 (2020).
Chowdhury, S. et al. Indian annual ambient air quality standard is achievable by completely mitigating emissions from household sources. Proc. Natl Acad. Sci. USA 116, 10711–10716 (2019).
Hajat, A., MacLehose, R. F., Rosofsky, A., Walker, K. D. & Clougherty, J. E. Confounding by socioeconomic status in epidemiological studies of air pollution and health: challenges and opportunities. Environ. Health Perspect. 129, 065001 (2021).
Krewski, D. et al. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res. Rep. Health Eff. Inst. 140, 5–114 (2009).
Clougherty, J. E. et al. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environ. Health Perspect. 115, 1140–1146 (2007).
Fuller, C. H., Feeser, K. R., Sarnat, J. A. & O’Neill, M. S. Air pollution, cardiovascular endpoints and susceptibility by stress and material resources: a systematic review of the evidence. Environ. Health 16, 58 (2017).
Hajat, A., Hsia, C. & O’Neill, M. S. Socioeconomic disparities and air pollution exposure: a global review. Curr. Environ. Health Rep. 2, 440–450 (2015).
Sun, X. et al. The associations between birth weight and exposure to fine particulate matter (PM2.5) and its chemical constituents during pregnancy: a meta-analysis. Environ. Pollut. 211, 38–47 (2016).
Reiss, R. et al. Evidence of health impacts of sulfate-and nitrate-containing particles in ambient air. Inhal. Toxicol. 19, 419–449 (2007).
Garçon, G. et al. Dunkerque City air pollution particulate matter-induced cytotoxicity, oxidative stress and inflammation in human epithelial lung cells (L132) in culture. Toxicol. In Vitro 20, 519–528 (2006).
Das, A., Habib, G., Vivekanandan, P. & Kumar, A. Reactive oxygen species production and inflammatory effects of ambient PM2.5 -associated metals on human lung epithelial A549 cells ‘one year-long study’: the Delhi chapter. Chemosphere 262, 128305 (2021).
Viehmann, A. et al. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup. Environ. Med 72, 656–663 (2015).
Trayhurn, P. & Wood, I. S. Signalling role of adipose tissue: adipokines and inflammation in obesity. Biochem. Soc. Trans. 33, 1078–1081 (2005).
Herter-Aeberli, I., Thankachan, P., Bose, B. & Kurpad, A. V. Increased risk of iron deficiency and reduced iron absorption but no difference in zinc, vitamin A or B-vitamin status in obese women in India. Eur. J. Nutr. 55, 2411–2421 (2016).
Dasi, T. et al. Point-of-care haemoglobin measurement in pooled capillary blood by a portable autoanalyser: comparison with venous blood haemoglobin measured by reference methods in cross-sectional and longitudinal studies. B. J. Nutr. 10, 1 (2021).
Petry, N. et al. The proportion of anemia associated with iron deficiency in low, medium, and high human development index countries: a systematic analysis of national surveys. Nutrients 8, 693 (2016).
National Nutrition Monitoring Bureau (NNMB) Diet and Nutritional Survey of Rural Population, Prevalence of Hypertension and Diabetes among Adults and Infant and Young Child Feeding Practices. Report of the Third Repeat Survey (NNMB, 2012).
Sanchis-Gomar, F., Cortell-Ballester, J., Pareja-Galeano, H., Banfi, G. & Lippi, G. Hemoglobin point-of-care testing: the HemoCue system. J. Lab. Autom. 18, 198–205 (2013).
Buchard, V. et al. The MERRA-2 aerosol reanalysis, 1980 onward. Part II: evaluation and case studies. J. Clim. 30, 6851–6872 (2017).
Jain, S., Sharma, S. K., Vijayan, N. & Mandal, T. K. Seasonal characteristics of aerosols (PM2.5 and PM10) and their source apportionment using PMF: a four year study over Delhi, India. Environ. Pollut. 262, 114337 (2020).
Skamarock, W. C. et al. A Description of the Advanced Research WRF Version 3 (No. NCAR/TN-475+STR) (University Corporation for Atmospheric Research, 2008).
Appel, K. W. et al. The Community Multiscale Air Quality (CMAQ) model versions 5.3 and 5.3.1: system updates and evaluation. Geosci. Model Dev. 14, 2867–2897 (2021).
Singh, N., Agarwal, S., Sharma, S., Chatani, S. & Ramanathan, V. Air pollution over India: causal factors for the high pollution with implications for mitigation. ACS Earth Space Chem. 5, 3297–3312 (2021).
Amann, M. et al. Cost-effective control of air quality and greenhouse gases in Europe: modeling and policy applications. Environ. Model. Softw. 26, 1489–1501 (2011).
Buchholz, R. R., Emmons, L. K., Tilmes, S. & the CESM2 Development Team. CESM2.1/CAM-chem Instantaneous Output for Boundary Conditions (UCAR/NCAR – Atmospheric Chemistry Observations and Modeling Laboratory, 2019).
Venkataraman, C. et al. Source influence on emission pathways and ambient PM2.5 pollution over India (2015–2050). Atmos. Chem. Phys. 18, 8017–8039 (2018).
Giglio, L., Randerson, J. T. & van der Werf, G. R. Analysis of daily, monthly, and annual burned area using the fourth-generation global fire emissions database (GFED4). J. Geophys. Res.: Biogeosci. 118, 317–328 (2013).
Li, M. et al. MIX: a mosaic Asian anthropogenic emission inventory under the international collaboration framework of the MICS-Asia and HTAP. Atmos. Chem. Phys. 17, 935–963 (2017).
Philip, S. et al. Spatially and seasonally resolved estimate of the ratio of organic mass to organic carbon. Atmos. Environ. 87, 34–40 (2014).
Kankaria, A., Nongkynrih, B. & Gupta, S. K. Indoor air pollution in India: implications on health and its control. Indian J. Community Med 39, 203–207 (2014).
Kyu, H. H., Georgiades, K. & Boyle, M. H. Biofuel smoke and child anemia in 29 developing countries: a multilevel analysis. Ann. Epidemiol. 20, 811–817 (2010).
Viana, M. B. Anemia and infection: a complex relationship. Rev. Bras. Hematol. Hemoter. 33, 90–92 (2011).
Acknowledgements
The work is supported by a research grant under the SUPRA scheme from the SERB, Department of Science and Technology, GoI. The exposure database was generated as part of a project under the NCAP funded by the Ministry of Environment, Forest and Climate Change, GoI. S.D. acknowledges financial support for the Institute Chair fellowship and DST-FIST programme (SR/FST/ESII-016/2014) for computing support. S.J. acknowledges the Institute Postdoctoral fellowship from IIT Delhi. S.W. acknowledges the National Natural Science Foundation of China (grant no. 22188102).
Author information
Authors and Affiliations
Contributions
S.D. and E.C. conceived the study and wrote the initial article. E.C. analysed the data with the help of S.G. S.S., N.S., S.A., S.W., C.V. and K.T. did the model simulations and analysis of the model outputs. A.V.K. and A.J.C. provided a critical review of aspects of the epidemiological analysis and aetiological frameworks. S.J. provided the PM2.5 composition data for validating the model data. All authors provided comments and contributed to the final version of the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Sustainability thanks Trenton Honda, Andrea Pozzer and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–9, discussion, Tables 1–4 and Notes 1 and 2.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chaudhary, E., Dey, S., Ghosh, S. et al. Reducing the burden of anaemia in Indian women of reproductive age with clean-air targets. Nat Sustain 5, 939–946 (2022). https://doi.org/10.1038/s41893-022-00944-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41893-022-00944-2
This article is cited by
-
A district-level geospatial analysis of anaemia prevalence among rural men in India, 2019-21
International Journal for Equity in Health (2024)
-
Cumulative effect of PM2.5 components is larger than the effect of PM2.5 mass on child health in India
Nature Communications (2023)
-
Soil micronutrients linked to human health in India
Scientific Reports (2023)
-
A Strategic Research Framework for Defeating Diabetes in India: A 21st-Century Agenda
Journal of the Indian Institute of Science (2023)
-
Particulates and anaemia in India
Nature Sustainability (2022)