Abstract
Impaired glucose-stimulated insulin secretion (GSIS) is a hallmark of type-2 diabetes. However, cellular signaling machineries that control GSIS remain incompletely understood. Here, we report that β-klotho (KLB), a single-pass transmembrane protein known as a co-receptor for fibroblast growth factor 21 (FGF21), fine tunes GSIS via modulation of glycolysis in pancreatic β-cells independent of the actions of FGF21. β-cell-specific deletion of Klb but not Fgf21 deletion causes defective GSIS and glucose intolerance in mice and defective GSIS in islets of type-2 diabetic mice is mitigated by adenovirus-mediated restoration of KLB. Mechanistically, KLB interacts with and stabilizes the cytokine receptor subunit GP130 by blockage of ubiquitin-dependent lysosomal degradation, thereby facilitating interleukin-6-evoked STAT3–HIF1α signaling, which in turn transactivates a cluster of glycolytic genes for adenosine triphosphate production and GSIS. The defective glycolysis and GSIS in Klb-deficient islets are rescued by adenovirus-mediated replenishment of STAT3 or HIF1α. Thus, KLB functions as a key cell-surface regulator of GSIS by coupling the GP130 receptor signaling to glucose catabolism in β-cells and represents a promising therapeutic target for diabetes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
The data supporting the findings of this study are available in source data files. Source data are provided with this paper.
References
Campbell, J. E. & Newgard, C. B. Mechanisms controlling pancreatic islet cell function in insulin secretion. Nat. Rev. Mol. Cell Biol. 22, 142–158 (2021).
Fu, Z., Gilbert, E. R. & Liu, D. Regulation of insulin synthesis and secretion and pancreatic β-cell dysfunction in diabetes. Curr. Diabetes Rev. 9, 25–53 (2013).
Butcher, M. J. et al. Association of proinflammatory cytokines and islet resident leucocytes with islet dysfunction in type 2 diabetes. Diabetologia 57, 491–501 (2014).
Deng, S. et al. Structural and functional abnormalities in the islets isolated from type 2 diabetic subjects. Diabetes 53, 624–632 (2004).
Marselli, L. et al. Are we overestimating the loss of β cells in type 2 diabetes? Diabetologia 57, 362–365 (2014).
Meier, J. J. & Bonadonna, R. C. Role of reduced β-cell mass versus impaired β-cell function in the pathogenesis of type 2 diabetes. Diabetes Care 36, S113–S119 (2013).
Del Guerra, S. et al. Functional and molecular defects of pancreatic islets in human type 2 diabetes. Diabetes 54, 727–735 (2005).
MacDonald, M. J. et al. Decreased levels of metabolic enzymes in pancreatic islets of patients with type 2 diabetes. Diabetologia 52, 1087–1091 (2009).
Li, X. et al. The MDM2-p53-pyruvate carboxylase signalling axis couples mitochondrial metabolism to glucose-stimulated insulin secretion in pancreatic β-cells. Nat. Commun. 7, 11740 (2016).
Lu, B. et al. Impaired β-cell glucokinase as an underlying mechanism in diet-induced diabetes. Dis. Model Mech. https://doi.org/10.1242/dmm.033316 (2018).
Geng, L., Lam, K.S.L. & Xu, A. The therapeutic potential of FGF21 in metabolic diseases: from bench to clinic. Nat. Rev. Endocrinol. https://doi.org/10.1038/s41574-020-0386-0 (2020).
Johnson, C. L. et al. Fibroblast growth factor 21 reduces the severity of cerulein-induced pancreatitis in mice. Gastroenterology 137, 1795–1804 (2009).
Coate, K. C. et al. FGF21 is an exocrine pancreas secretagogue. Cell Metab. 25, 472–480 (2017).
Wente, W. et al. Fibroblast growth factor-21 improves pancreatic β-cell function and survival by activation of extracellular signal-regulated kinase 1/2 and Akt signaling pathways. Diabetes 55, 2470–2478 (2006).
Singhal, G. et al. Fibroblast growth factor 21 (FGF21) protects against high fat diet induced inflammation and islet hyperplasia in pancreas. PLoS ONE 11, e0148252 (2016).
Xu, J. et al. Acute glucose-lowering and insulin-sensitizing action of FGF21 in insulin-resistant mouse models–association with liver and adipose tissue effects. Am. J. Physiol. Endocrinol. Metab. 297, E1105–E1114 (2009).
Ogawa, Y. et al. β-Klotho is required for metabolic activity of fibroblast growth factor 21. Proc. Natl Acad. Sci. USA 104, 7432–7437 (2007).
Kurosu, H. et al. Tissue-specific expression of β-klotho and fibroblast growth factor (FGF) receptor isoforms determines metabolic activity of FGF19 and FGF21. J. Biol. Chem. 282, 26687–26695 (2007).
Ito, S. et al. Molecular cloning and expression analyses of mouse β-klotho, which encodes a novel klotho family protein. Mechanisms Dev. 98, 115–119 (2000).
Fon Tacer, K. et al. Research resource: comprehensive expression atlas of the fibroblast growth factor system in adult mouse. Mol. Endocrinol. 24, 2050–2064 (2010).
Ding, X. et al. β-Klotho is required for fibroblast growth factor 21 effects on growth and metabolism. Cell Metab. 16, 387–393 (2012).
Owen, B. M. et al. FGF21 acts centrally to induce sympathetic nerve activity, energy expenditure, and weight loss. Cell Metab. 20, 670–677 (2014).
So, W. Y. et al. High glucose represses β-klotho expression and impairs fibroblast growth factor 21 action in mouse pancreatic islets: involvement of peroxisome proliferator-activated receptor γ signaling. Diabetes 62, 3751–3759 (2013).
Geng, L. et al. Exercise alleviates obesity-induced metabolic dysfunction via enhancing FGF21 sensitivity in adipose tissues. Cell Rep. 26, 2738–2752 (2019).
Roider, H. G., Manke, T., O’Keeffe, S., Vingron, M. & Haas, S. A. PASTAA: identifying transcription factors associated with sets of co-regulated genes. Bioinformatics 25, 435–442 (2009).
Cantley, J., Grey, S. T., Maxwell, P. H. & Withers, D. J. The hypoxia response pathway and β-cell function. Diabetes, Obes. Metab. 12, 159–167 (2010).
Lau, H. H., Ng, N. H. J., Loo, L. S. W., Jasmen, J. B. & Teo, A. K. K. The molecular functions of hepatocyte nuclear factors: in and beyond the liver. J. Hepatol. 68, 1033–1048 (2018).
Cheng, K. et al. Hypoxia-inducible factor-1α regulates β cell function in mouse and human islets. J. Clin. Invest. 120, 2171–2183 (2010).
Masoud, G. N. & Li, W. HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharm. Sin. B 5, 378–389 (2015).
Jung, J. E. et al. STAT3 inhibits the degradation of HIF-1α by pVHL-mediated ubiquitination. Exp. Mol. Med. 40, 479–485 (2008).
Pawlus, M. R., Wang, L. & Hu, C. J. STAT3 and HIF1α cooperatively activate HIF1 target genes in MDA-MB-231 and RCC4 cells. Oncogene 33, 1670–1679 (2014).
Jung, J. E. et al. STAT3 is a potential modulator of HIF-1-mediated VEGF expression in human renal carcinoma cells. FASEB J. 19, 1296–1298 (2005).
Gorogawa, S. et al. Insulin secretory defects and impaired islet architecture in pancreatic β-cell-specific STAT3 knockout mice. Biochem. Biophys. Res. Commun. 319, 1159–1170 (2004).
Bromberg, J. F. et al. Stat3 as an oncogene. Cell 98, 295–303 (1999).
Vallania, F. et al. Genome-wide discovery of functional transcription factor binding sites by comparative genomics: the case of Stat3. PNAS 106, 5117–5122 (2009).
Zhong, Z., Wen, Z. & Darnell, J. E. Jr. Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science 264, 95–98 (1994).
Zhang, F., Chen, Y., Heiman, M. & Dimarchi, R. Leptin: structure, function and biology. Vitam. Hormones 71, 345–372 (2005).
Qing, H. et al. Origin and function of stress-induced IL-6 in murine models. Cell 182, 372–387 (2020).
Kristiansen, O. P. & Mandrup-Poulsen, T. Interleukin-6 and diabetes: the good, the bad, or the indifferent? Diabetes 54, S114–S124 (2005).
Jones, S. A., Scheller, J. & Rose-John, S. Therapeutic strategies for the clinical blockade of IL-6/gp130 signaling. J. Clin. Invest. 121, 3375–3383 (2011).
Tanaka, Y. et al. c-Cbl-dependent monoubiquitination and lysosomal degradation of gp130. Mol. Cell. Biol. 28, 4805–4818 (2008).
Liu, H. et al. E3 ubiquitin ligase NEDD4L negatively regulates keratinocyte hyperplasia by promoting GP130 degradation. EMBO Rep. 22, e52063 (2021).
Kershaw, N. J., Laktyushin, A., Nicola, N. A. & Babon, J. J. Reconstruction of an active SOCS3-based E3 ubiquitin ligase complex in vitro: identification of the active components and JAK2 and gp130 as substrates. Growth Factors 32, 1–10 (2014).
Degirolamo, C., Sabba, C. & Moschetta, A. Therapeutic potential of the endocrine fibroblast growth factors FGF19, FGF21 and FGF23. Nat. Rev. Drug Discov. 15, 51–69 (2016).
Hotta, Y. et al. Fibroblast growth factor 21 regulates lipolysis in white adipose tissue but is not required for ketogenesis and triglyceride clearance in liver. Endocrinology 150, 4625–4633 (2009).
Dutchak, P. A. et al. Fibroblast growth factor-21 regulates PPARγ activity and the antidiabetic actions of thiazolidinediones. Cell 148, 556–567 (2012).
Tanner, L. B. et al. Four key steps control glycolytic flux in mammalian cells. Cell Syst. 7, 49–62.e48 (2018).
Gunton, J. E. et al. Loss of ARNT/HIF1β mediates altered gene expression and pancreatic-islet dysfunction in human type 2 diabetes. Cell 122, 337–349 (2005).
Rudland, V. L. Diagnosis and management of glucokinase monogenic diabetes in pregnancy: current perspectives. Diabetes Metab. Syndr. Obes. 12, 1081–1089 (2019).
Lee, J. W., Bae, S. H., Jeong, J. W., Kim, S. H. & Kim, K. W. Hypoxia-inducible factor (HIF-1)α: its protein stability and biological functions. Exp. Mol. Med. 36, 1–12 (2004).
Carlsson, P. O., Liss, P., Andersson, A. & Jansson, L. Measurements of oxygen tension in native and transplanted rat pancreatic islets. Diabetes 47, 1027–1032 (1998).
Cantley, J. et al. Deletion of the von Hippel–Lindau gene in pancreatic β cells impairs glucose homeostasis in mice. J. Clin. Invest. 119, 125–135 (2009).
Puri, S., Cano, D. A. & Hebrok, M. A role for von Hippel–Lindau protein in pancreatic β-cell function. Diabetes 58, 433–441 (2009).
Zehetner, J. et al. PVHL is a regulator of glucose metabolism and insulin secretion in pancreatic β cells. Genes Dev. 22, 3135–3146 (2008).
Carlsson, P. O., Palm, F., Andersson, A. & Liss, P. Markedly decreased oxygen tension in transplanted rat pancreatic islets irrespective of the implantation site. Diabetes 50, 489–495 (2001).
Miao, G. et al. Dynamic production of hypoxia-inducible factor-1α in early transplanted islets. Am. J. Transplant. 6, 2636–2643 (2006).
Juang, J. H., Hsu, B. R., Kuo, C. H. & Ueng, S. W. Beneficial effects of hyperbaric oxygen therapy on islet transplantation. Cell Transplant. 11, 95–101 (2002).
Schofield, C. J. & Ratcliffe, P. J. Oxygen sensing by HIF hydroxylases. Nat. Rev. Mol. Cell Biol. 5, 343–354 (2004).
Gao, W. et al. Hypoxia and STAT3 signalling interactions regulate pro-inflammatory pathways in rheumatoid arthritis. Ann. Rheum. Dis. 74, 1275–1283 (2015).
Kim, B. G. et al. Aberrant activation of signal transducer and activator of transcription-3 (STAT3) signaling in endometriosis. Hum. Reprod. 30, 1069–1078 (2015).
Carey, A. L. & Febbraio, M. A. Interleukin-6 and insulin sensitivity: friend or foe? Diabetologia 47, 1135–1142 (2004).
Ostrowski, K., Rohde, T., Zacho, M., Asp, S. & Pedersen, B. K. Evidence that interleukin-6 is produced in human skeletal muscle during prolonged running. J. Physiol. 508, 949–953 (1998).
Paula, F. M. et al. Exercise increases pancreatic β-cell viability in a model of type 1 diabetes through IL-6 signaling. FASEB J. 29, 1805–1816 (2015).
Ellingsgaard, H. et al. Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and α cells. Nat. Med. 17, 1481–1489 (2011).
Senn, J. J., Klover, P. J., Nowak, I. A. & Mooney, R. A. Interleukin-6 induces cellular insulin resistance in hepatocytes. Diabetes 51, 3391 (2002).
Skiniotis, G., Boulanger, M. J., Garcia, K. C. & Walz, T. Signaling conformations of the tall cytokine receptor gp130 when in complex with IL-6 and IL-6 receptor. Nat. Struct. Mol. Biol. 12, 545–551 (2005).
Heinrich, P. C. et al. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochemical J. 374, 1–20 (2003).
Fasnacht, N. & Müller, W. Conditional gp130-deficient mouse mutants. Semin. Cell Dev. Biol. 19, 379–384 (2008).
Flynn, C. M. et al. Interleukin-6 controls recycling and degradation, but not internalization of its receptors. J. Biol. Chem. 296, 100434 (2021).
Shi, Y. et al. Tetraspanin CD9 stabilizes gp130 by preventing its ubiquitin-dependent lysosomal degradation to promote STAT3 activation in glioma stem cells. Cell Death Differ. 24, 167–180 (2017).
Grabbe, C., Husnjak, K. & Dikic, I. The spatial and temporal organization of ubiquitin networks. Nat. Rev. Mol. Cell Biol. 12, 295–307 (2011).
White, U. A. & Stephens, J. M. The gp130 receptor cytokine family: regulators of adipocyte development and function. Curr. Pharm. Des. 17, 340–346 (2011).
Rocheleau, J. V., Head, W. S., Nicholson, W. E., Powers, A. C. & Piston, D. W. Pancreatic islet β-cells transiently metabolize pyruvate. J. Biol. Chem. 277, 30914–30920 (2002).
Wang, B. et al. Activation of hypothalamic RIP-Cre neurons promotes beiging of WAT via sympathetic nervous system. EMBO Rep. https://doi.org/10.15252/embr.201744977 (2018).
Jimenez-Moreno, C. M. et al. A simple high efficiency intra-islet transduction protocol using lentiviral vectors. Curr. Gene Ther. 15, 436–446 (2015).
Kong, Y., Ebrahimpour, P., Liu, Y., Yang, C. & Alonso, L.C. Pancreatic islet embedding for paraffin sections. J. Vis. Exp. https://doi.org/10.3791/57931 (2018).
Acknowledgements
This work was supported by the General Research Fund (17121819, A.M.X.) and Area of Excellence (AOE/M/707-18, A.M.X.) from the Research Grant Council of Hong Kong, the National Natural Science Foundation of China (82070860, A.M.X. and 32000816, L.L.G.) and Hong Kong Health and Medical Research Fund (06172956, Q.Z.L.). Y.T.Z. was supported by the Natural Science Foundation of Guangdong Province (2017A030307001).
Author information
Authors and Affiliations
Contributions
L.L.G. designed the study, carried out the research, analyzed and interpreted the results and wrote the manuscript. B.Y.L. carried out the research and data analysis. L.G.J., X.Y.Z., B.L.W. and J.L. helped with the molecular, cellular and biochemical experiments. J.S.Y. helped data analysis and drawing the schematic diagrams. Y.T.Z. and L.Z. helped with the animal experiments. J.F.L. and W.J. helped with the analysis of glycolytic metabolites. J.K.Y. helped with human islet study. Q.Z.L. advised the study and edited the manuscript. A.M.X. conceived and supervised the study, wrote and edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Metabolism thanks Marc Donath and the other, anonymous, reviewers for their contribution to the peer review of this work. Primary handling editor: Isabella Samuelson, in collaboration with the Nature Metabolism team
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 FGF21 has no obvious effects on GSIS.
a, Illustration of the experimental design for the effects of recombinant mouse FGF21 (rmFGF21) protein on GSIS in islets isolated from 20-week-old male C57BL/6J lean, diet-induced obese (DIO, fed with a high-fat diet for 12 weeks) and db/db mice. b, Insulin secretion capacities of isolated islets treated with 50 nM rmFGF21 protein for 0-72 h under 2.8 mM or 16.7 mM glucose condition (n = 6 mice). c, Insulin secretion capacities of isolated islets treated with rmFGF21 protein at 0, 50, 100 nM for 48 h under 2.8 mM or 16.7 mM glucose condition (n = 6 mice). d, Islets isolated from lean, DIO and db/db mice were fasted for 12 h and treated with 0, 50, 100 nM rmFGF21 protein for 10 min, followed by examination of p-Erk (Thr202/Tyr204) and t-Erk protein levels by Western blot. Similar results were obtained from three independent experiments. e, Rat INS-1E (n = 6 independent cultures) and mouse MIN6 β-cells (n = 7 independent cultures) were treated with 0, 50, 100 nM rmFGF21 protein for 48 h before exposure to 2.8 mM or 16.7 mM glucose for 30 min. Insulin concentration in the conditioned medium was measured and normalized to cell protein concentrations. f-g, Blood glucose levels (f) and serum insulin levels (g) in male 14-week-old WT (FGF21+/+) and Fgf21 KO (FGF21-/-) mice under feeding or fasting conditions (n = 8 mice). h-i, GTT (h, n = 8 mice) and GSIS (i, n = 6 mice) were performed in male FGF21+/+ and FGF21-/- mice on regular diet for 12 weeks and the values of area under curve (AUC) were quantified. j, Dynamic insulin secretion under basal or high glucose condition was measured in cultured islets isolated from male FGF21+/+ and FGF21-/- mice on regular diet for 12 weeks (n = 6 mice). Data are presented as mean ± SEM.
Extended Data Fig. 2 Effects of β-cell-selective deletion of Klb in mice.
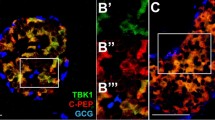
a, Daily food intake in KlbF/F, KlbRIP and RIP-Cre mice on STC diet for 12 weeks (n = 5 mice for KlbF/F group, n = 6 mice for KlbRIP group, n = 5 for RIP-Cre group). b-c, Body weight and composition in KlbF/F, KlbRIP and RIP-Cre mice on STC diet for 16 weeks (b, n = 6 mice for each group) or HFD for 12 weeks (c, n = 7 mice for KlbF/F group, n = 7 mice for KlbRIP group, n = 8 mice for RIP-Cre group). d-e. Insulin tolerance test (ITT) in KlbF/F, KlbRIP and RIP-Cre mice on STC feeding for 15 weeks (d) or HFD for 11 weeks (e) (n = 6 mice). f, Representative H&E staining of pancreatic sections of STC- and HFD-fed KlbF/F, KlbRIP and RIP-Cre mice. The islets were circled with blue lines. Similar results were obtained from three independent experiments. Scale bar, 50μm. g, Representative immunofluorescence staining of glucagon (red) and insulin (green) in pancreatic sections of STC- and HFD-fed KlbF/F, KlbRIP and RIP-Cre mice. Similar results were obtained from three independent experiments. Scale bar, 50μm. h, The β-cell mass in STC- and HFD-fed KlbF/F, KlbRIP and RIP-Cre mice (n = 7 mice). i, Relative mRNA levels of β-cell marker genes in islets isolated from STC-fed KlbF/F, KlbRIP and RIP-Cre mice (n = 8 mice). Data are presented as mean ± SEM.
Extended Data Fig. 3 Restoration of KLB expression alleviates defective GSIS in islets isolated from db/db mice.
a, Representative immunoblots and quantification of KLB in islets isolated from C57BL/6J mice fed with STC or HFD for 16 weeks (n = 8 mice). b, Correlation between GSIS capacity and Klb mRNA level in islets isolated from C57BL/6J mice fed with STC or HFD for 16 weeks (n = 16 mice). c, Representative immunoblots and quantification of KLB in islets isolated from 16-week-old C57BKS m + /db and db/db mice (n = 8 mice). d, Correlation between GSIS capacity and the Klb mRNA level in islets isolated from 16-week-old C57BKS m + /db or db/db mice (n = 16 mice). e, Illustration of the experimental design to evaluate the effect of adenovirus-mediated expression of KLB on insulin secretion in diabetic islets. f, Representative microscopic examination of GFP signals in cultured islets infected with various adenoviruses by paraffin sectioning. Similar results were obtained from three independent experiments. Scale bar, 50μm. g, Representative immunoblots of KLB and Tubulin in islets infected with indicated adenoviruses. Similar results were obtained from three independent experiments. h, Dynamic GSIS and quantification of AUC in islets at 48 h after adenovirus infection (n = 6 mice). i-j, Glycolytic flux measured by 3H2O generated from [5-3H]-glucose (i, n = 8 mice) and ATP production (j, n = 6 mice) in isolated islets infected with indicated adenoviruses. Data are presented as mean ± SEM. P values are derived from two-tailed unpaired t-test with Welch’s correction (a, c), two-tailed nonparametric Spearman correlation (b, d), Welch’s ANOVA followed by Dunnett’s T3 multiple comparisons test (h), or ordinary two-way ANOVA followed by Tukey’s multiple-comparisons test (i, j).
Extended Data Fig. 4 AAV-mediated depletion of KLB in pancreatic β-cells of adult mice impairs glucose uptake and glycolysis.
Islets were isolated from 16-week-old KlbF/F mice injected with AAV–RIP-GFP or AAV–RIP-Cre, or C57BL/6 J mice injected with AAV–RIP-Cre as described in Fig. 1l. a, Glycolytic flux measured by 3H2O generated from [5-3H]-glucose through glycolysis (n = 8 mice for each group). b, Glucose uptake measured by radioisotope-labeled glucose analog 3H-2-deoxyglucose assay (n = 8 mice for KlbF/F-GFP group, n = 8 mice for KlbF/F-Cre group, n = 7 mice for C57-Cre group). c, Enzymatic activities of hexokinase (HK), phosphofructokinase (PFK), pyruvate kinase (PK) (n = 7 mice for each group). Data are presented as mean ± SEM. P values are derived from ordinary two-way ANOVA followed by Tukey’s multiple-comparisons test (a, c), or ordinary one-way ANOVA followed by Tukey’s multiple-comparisons test (b).
Extended Data Fig. 5 Excessive overexpression of HIF1α is not able to rescue defective GSIS in Klb-null β-cells.
Islets isolated from 16-week-old male KlbRIP or KlbF/F mice were infected with adenovirus encoding Myc-tagged HIF1α (Adv-HIF1α) or GFP (Adv-GFP) at 300 multiplicity of infection (MOI) for 24 h. a, Representative immunoblots with anti-HIF1α, Myc, GFP or Tubulin antibodies in isolated islets infected with different adenoviruses (left) and quantification of HIF1α protein levels normalized to Tubulin (right, n = 6 mice). b-e, Insulin secretion (b, n = 8 mice), glycolytic flux measured by 3H2O generated from [5-3H]-glucose (c, n = 8 mice), mitochondrial TCA flux measured by 14CO2 generated from [2-14C]-pyruvate (d, n = 8 mice for KlbF/F-GFP, n = 8 mice for KlbRIP-GFP group, n = 9 mice for KlbRIP-HIF1α group) and ATP production (e, n = 6 mice) under basal (2.8 mM glucose) or high-glucose (16.7 mM) conditions in isolated islets infected with different adenoviruses. Data are presented as mean ± SEM. P values are derived from Welch’s ANOVA followed by Dunnett’s T3 multiple comparisons test (a), or ordinary two-way ANOVA followed by Tukey’s multiple-comparisons test (b-e).
Extended Data Fig. 6 STAT3 modulates HIF1α expression and GSIS in β-cells.
a, Phosphorylation and expression levels of several kinases and transcription factors in islets isolated from 16-week-old male KlbF/F and KlbRIP mice as determined by immunoblotting (n = 4 mice for each group). b, Mouse MIN6 β-cells were infected with adenovirus encoding GFP (Adv-GFP) or Flag-tagged constitutively active STAT3 (Adv-STAT3c) at 100 MOI for 48 h, followed by examination of insulin secretion under 2.8 mM or 16.7 mM glucose conditions. The insulin secretion capacities were normalized to the cell protein concentration (n = 7 independent cultures). c, Mouse MIN6 β-cells were treated with the STAT3 inhibitor S3I-201 (200 μM) or PBS for 24 h, followed by immunoblotting analysis of p-STAT3, t-STAT3, HIF1α and Tubulin (left). The expression levels of HIF1α protein were quantified by densitometry analysis (right, n = 6 independent cultures). d, Basal (2.8 mM glucose) and high glucose (16.7 mM)-stimulated insulin secretion capacities were assessed in cells described in panel c (n = 7 independent cultures). e, ChIP assays with a rabbit anti-p-STAT3(Tyr705) polyclonal antibody were performed in islets isolated from 15-week-old male KlbF/F and KlbRIP mice using primers spanning to the SIE1 and SIE2 regions within the mouse Hif1α proximal promoters as described in Fig. 6e. The precipitated chromatin was quantified by real-time PCR and the relative fold change was calculated by normalizing to the genomic 36b4 gene (n = 8 mice for KlbF/F group, n = 9 mice for KlbRIP group). Data are presented as mean ± SEM. P values are derived from ordinary two-way ANOVA followed by Sidak’s multiple comparisons test (b, d, e), or two-tailed unpaired t-test (c).
Extended Data Fig. 7 Effects of excessive IL6 treatment on glucose control and insulin secretion in mice.
a-d, Schematic diagram of chronic rmIL6 protein administration (a). 15-week-old male KlbF/F and KlbRIP mice were administered with rmIL6 protein (0.2 mg/kg/day) or PBS for 10 days. The blood was collected from tail vein to measure the circulating IL6 concentration every other day (b, n = 4 mice for each group). On the last day, GTT was performed (c, n = 8 mice for each group) and serum insulin levels were measured to assess GSIS (d, n = 6 mice for each group). Data are presented as mean ± SEM. P values are derived from ordinary two-way ANOVA followed by Sidak’s multiple comparisons test (c-d).
Extended Data Fig. 8 Overexpression of degradation-resistant GP130 reverses impaired GSIS and glycolysis in KlbRIP islets.
a, Islets isolated from male 16-week-old KlbF/F or KlbRIP mice were infected with adenovirus encoding Flag-tagged GP130 with K716R mutation or GFP at 100 multiplicity of infection (MOI) for 24 h. b, Representative immunoblots with anti-GP130, GFP, Flag or Tubulin antibodies in isolated islets infected with different adenoviruses. Similar results were obtained from three independent experiments. c-d, Insulin secretion (c) and glycolytic flux measured by 3H2O generated from [5-3H]-glucose (d) under 2.8 mM or 16.7 mM glucose conditions in isolated islets infected with different adenoviruses (n = 7 mice for each group). e, Immunoblots for p-STAT3(Tyr705) and t-STAT3 in islets infected with different adenoviruses (upper) and densitometric quantification of the relative expression levels of p-/t-STAT3 (lower, n = 4 mice for each group). f, Relative expression levels of Hif1α and glycolytic genes quantified by real-time PCR and normalized to β-actin gene in islets infected with different adenoviruses. The mRNA level in KlbF/F-GFP group was set as 1 (n = 8 mice for each group). Data are presented as mean ± SEM. P values are derived from ordinary two-way ANOVA followed by Tukey’s multiple-comparisons test (c, d) or ordinary one-way ANOVA followed by Tukey’s multiple-comparisons test (e).
Extended Data Fig. 9 Working model for an FGF21-independent role of KLB in regulating insulin secretion.
KLB interacts with GP130 and prevents ubiquitin-dependent lysosomal degradation of GP130, thereby facilitating IL6-induced STAT3–HIF1α signaling to maintain normal glycolysis and GSIS in pancreatic β-cells.
Supplementary information
Supplementary Information
Supplementary Figs. 1–6 and Supplementary Tables 1–3.
Supplementary Data 1
Statistical source data for Supplementary Figs. 1–4.
Source data
Source Data Fig. 1
Statistical Source Data.
Source Data Fig. 1
Unprocessed western blots.
Source Data Fig. 2
Statistical Source Data.
Source Data Fig. 3
Statistical Source Data.
Source Data Fig. 3
Unprocessed western blots.
Source Data Fig. 4
Statistical Source Data.
Source Data Fig. 4
Unprocessed western blots.
Source Data Fig. 5
Statistical Source Data.
Source Data Fig. 5
Unprocessed western blots.
Source Data Fig. 6
Statistical Source Data.
Source Data Fig. 6
Unprocessed western blots.
Source Data Fig. 7
Statistical Source Data.
Source Data Fig. 7
Unprocessed western blots.
Source Data Fig. 8
Statistical Source Data.
Source Data Fig. 8
Unprocessed western blots.
Source Data Extended Data Fig. 1
Statistical Source Data.
Source Data Extended Data Fig. 1
Unprocessed western blots.
Source Data Extended Data Fig. 2
Statistical Source Data.
Source Data Extended Data Fig. 3
Statistical Source Data.
Source Data Extended Data Fig. 3
Unprocessed western blots.
Source Data Extended Data Fig. 4
Statistical Source Data.
Source Data Extended Data Fig. 5
Statistical Source Data.
Source Data Extended Data Fig. 5
Unprocessed western blots.
Source Data Extended Data Fig. 6
Statistical Source Data.
Source Data Extended Data Fig. 6
Unprocessed western blots.
Source Data Extended Data Fig. 7
Statistical Source Data.
Source Data Extended Data Fig. 8
Statistical Source Data.
Source Data Extended Data Fig. 8
Unprocessed western blots.
Rights and permissions
About this article
Cite this article
Geng, L., Liao, B., Jin, L. et al. β-Klotho promotes glycolysis and glucose-stimulated insulin secretion via GP130. Nat Metab 4, 608–626 (2022). https://doi.org/10.1038/s42255-022-00572-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42255-022-00572-2
This article is cited by
-
Periodontitis as a promoting factor of T2D: current evidence and mechanisms
International Journal of Oral Science (2023)
-
Baicalein Attenuates Neuroinflammation in LPS-Treated BV-2 Cells by Inhibiting Glycolysis via STAT3/c-Myc Pathway
Neurochemical Research (2023)