Abstract
Study Design:
Prospective cross-sectional study.
Objectives:
To investigate the timing of deep vein thrombosis (DVT) onset secondary to spinal cord injury without anticoagulant therapies.
Setting:
Spinal Cord Injury Center in Hokkaido, Japan.
Methods:
Between November 2012 and June 2013, patients with spinal cord injury who were admitted to our hospital within 1 day after the injury and treated surgically within 24 h underwent a neurological examination, leg vein ultrasonography and D-dimer test 1, 3, 7, 14 and 28 days after surgery. All patients received treatment with intermittent pneumatic compression and elastic stockings, but without any anticoagulant.
Results:
DVT developed in 12 patients (11 men and 1 women), with a mean age of 62.2 years (range, 41–80 years; mean age of total sample, 63.2 years (range, 25–78 years)), all distal to the popliteal vein. DVT occurred more often with a more severe paralysis (66.3%, AIS A and B). The median (± standard error) length of time from the operation to DVT detection was 7.5±2.2 days. The mean D-dimer level upon DVT detection was 14.6±11.8 μg ml−1, with no significant differences between those who developed DVT and those who did not at any of the time points.
Conclusion:
These results suggest that DVT can develop at the very-acute stage of spinal cord injury and the incidence increases with a more severe paralysis. DVT detection was more reliable with ultrasonography, which should be used with DVT-preventive measures, beginning immediately after the injury, for the management of patients with spinal cord injury.
Similar content being viewed by others
Introduction
Deep vein thrombosis (DVT) is one of the most dangerous complications of a spinal cord injury. DVT has a high incidence in patients with spinal cord injury as compared with patients with other diseases1 with a high mortality rate if complicated by pulmonary embolism.2
Although prevention, early detection and timely treatment of DVT are important during the management of patients with spinal cord injury, the timing of DVT onset secondary to a spinal cord injury has not yet been determined. In order to clarify these problems, this study aimed to investigate the timing of DVT onset by prospectively analyzing the patients immediately after a spinal cord injury.
Materials and methods
A prospective study was conducted in all patients with spinal cord injury admitted to our hospital between November 2012 and June 2013 within 1 day after the injury and treated surgically within 24 h. A neurological examination, leg vein ultrasonography and clotting system test (D-dimer) was performed 1, 3, 7, 14 and 28 days after surgery. Leg vein ultrasonography was carried out by using an Aplio XG (TOSHIBA, Tokyo, Japan) by experienced sonographers.
Intermittent pneumatic compression (IPC) with a calf pump (Kendall SCD EXPRESS, COVIDINE, Dublin, Ireland) and elastic stockings (ES) were used in all cases. The patient were kept foot pump attached throughout the day (except when the patient left the bed) for at least 2 consecutive weeks. The use of ES began on the day after the operation, as far as possible, with a median of 3 days between the operation and their use. Patients were advised to keep them on, except when bathing. One patient refused to wear them, and two patients had difficulty wearing them because of skin irritation. The other patients continued to use them until discharge from the hospital.
As a rule, we allowed the patients to leave the bed by using a wheelchair from the day after the surgery, with a median (± standard error) of 3±0.7 days from the surgery. Ten patients were unable to leave their bed on the day after the operation because of elective surgery (six cases), mechanical ventilation (two cases) and chest tube (two cases).
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
The sample included 25 men and 4 women with a mean age of 63.2 years (25–78 years). The spinal cord injury occurred at the cervical segment in 19 cases and thoracic/lumbar segment in 10 cases. The cause of spinal cord injury was a fall from a great height in 11 cases, fall from a low height in 2 cases, same-level fall in 8 cases, traffic accident in 4 cases, fall from a staircase in 1 case and sports accident in 3 cases. The median period from injury to hospitalization was 0 day (0–1 day). Twenty-four patients were admitted to our hospital on the day of the injury and 5 were hospitalized on the following day. The severity of paralysis at admission (American Spinal Cord Association (ASIA) Impairment Scale (AIS)) was A in 9 cases, B in 2 cases, C in 8 cases and D in 10 cases. The paralyzed level (ASIA Neurological Level of Injury (NLI)) was C3–4 in 11 cases, C5–8 in 8 cases, T1–12 in 6 cases and L1–4 in 4 cases. DVT developed in 12 patients (41.4%; 11 men and 1 woman), with a mean age of 62.2 years (range, 41–80 years). In all of these cases, the DVT was located distal to the popliteal vein. DVT affected both sides in 2 cases, the left side in 5 cases and the right side in 5 cases. Among these 12 patients, the injured level was the cervical segment in 7 cases and thoracic/lumbar segment in 5 cases, and the paralyzed level according to the NLI classification was C3–4 in 4 cases, C5–8 in 2 cases, T1–12 in 3 cases and L1–4 in 3 cases. The severity of paralysis (AIS) was A in 7 (58.3%) of these 12 cases, B in 1 case (8.3%), C in 3 cases (25.0%) and D in 1 case (8.3%). Thus, DVT occurred more often with paralysis of AIS grades A and B (complete motor paralysis) than with a partial motor paralysis (Tables 1a and b). DVT was detected on postoperative day 3 in 3 cases (25.0%), postoperative day 7 in 5 cases (41.7%), postoperative day 14 in 1 case (8.3%) and postoperative day 28 in 3 cases (25.0%). The median length of time from the operation to DVT detection was 7.5±2.2 days (± standard error) (Table 2).
The mean D-dimer level at DVT detection was 14.6±13.5 μg ml−1 (range, 2.78–44.3 μg ml−1). There was no significant difference between the DVT negative group and DVT positive group in terms of D-dimer level upon admission or on postoperative day 1, 3, 7, 14 or 28 (Mann–Whitney test, P=0.117, 0.059, 0.028, 0.075, 0.306 and 0.124, respectively).
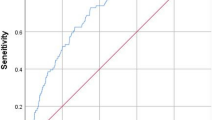
The cutoff D-dimer levels determined from the receiver operator characteristic (ROC) curve was 7.34, 7.88, 5.82, 10.99, 11.44, and 5.88 at admission and on the postoperative days 1, 3, 7, 14 and 28, respectively. The sensitivity/specificity (%) at these points of time were 75.0/70.6, 41.7/94.1, 72.7/76.5, 55.6/88.2, 60.0/93.3 and 75.0/93.3, respectively (Table 3).
Discussion
Timing and incidence of DVT in spinal cord injury patients
Concerning the pathogenesis of DVT, the three major factors in Virchow’s triad (blood retention, capillary wall disorder and blood coagulopathy) are well known.3 After spinal cord injury, paralysis is accompanied by reduced vascular contraction (because of a sympathetic nerve disorder) and reduced venous return (because of disturbed muscle contraction), leading to blood retention.4 Furthermore, a possible loss of the circadian variation in hemostatic and fibrinolytic function has also been suggested in patients with spinal cord injury. Thus, DVT is quite likely to develop in the presence of spinal cord injury. Considering the known mechanisms for the onset of DVT, we need to bear in mind that the risk for DVT increases with more severe paralysis and the incidence of DVT is particularly high in patients with complete motor paralysis associated with spinal cord injury.5, 6 In other words, the incidence of DVT is high in paralyzed patients with spinal cord injury; therefore, early detection and treatment are essential in such cases.
For early detection, we need to understand the timing associated with DVT onset; however, we have little information regarding the timing of DVT onset. In a retrospective analysis of 52 patients, Sugimoto et al.7 reported that they observed DVT 2–13 days after injury of the cervical segment of the spinal cord, suggesting that DVT can develop soon after spinal cord injury. To the best of our knowledge, the present study is the first to prospectively document the timing of DVT onset in patients with a spinal cord injury, with analysis commencing immediately after their injury. We detected no DVT positive patient on Day 1 but 3 patients were positive on Day 3, 5 on Day 7, 1 on Day 14 and 3 on Day 28.
As a result, DVT was detected 3 days after injury in 25% of the patients who developed DVT. Especially in the group of AIS A as complete paralysis, DVT occurred in 78% of patients. These findings indicate that proactive DVT prevention and diagnosis, beginning immediately after the injury, are indispensable in the management of the patients with a spinal cord injury.
How to diagnose DVT in spinal cord injury patients
D-dimer measurement and leg ultrasonography are predominantly used for the diagnosis of DVT. However, according to a study of patients who developed DVT after total knee or hip replacement surgery, both the sensitivity and specificity of D-dimer are low, indicating that D-dimer alone does not provide a sufficient means of DVT diagnosis.8, 9 Similar results were obtained in the present study, and the D-dimer level varied depending on the timing of the measurement, indicating a limitation in the accuracy of diagnosis based on D-dimer levels. DVT-inducing pulmonary embolism is a potentially fatal complication, and it seems advisable to use D-dimer only as an auxiliary indicator.
Diagnostic reliability is highest with leg ultrasonography. The sensitivity of ultrasonography in detecting leg DVT is reported to be 98–100% and its specificity to be 75–100%.10, 11, 12 This is an excellent method for the noninvasive screening of DVT.13 Shortcomings of this modality include the amount of time and labor required. For spinal cord injury accompanied by paralysis, periodic leg ultrasonography is indispensable. The results of the present study suggest that frequent leg ultrasonography, beginning immediately after injury, is needed for patients with severe paralysis (AIS A-C).
Prevention of DVT
In patients with a spinal cord injury, the incidence of DVT is quite high, and active measures for prevention are important, beginning from the acute stage of injury.1 The basic principles for DVT prevention include the prevention of venous retention, stimulation of venous return, and anticoagulation, with the use of ES, IPC and low-dose unfractionated heparin (LDUH), respectively. In the present study, ES and IPC were used immediately after injury, but this approach could not prevent DVT from occurring. These results indicate that it is necessary to include LDUH in the treatment of paralyzed patients with spinal cord injury. However, since patients with spinal cord injury often have hemorrhaging around the spine or spinal cord, physicians are often cautious about the use of LDUH because bleeding inside/outside the spinal cord is likely to aggravate the paralysis.
Recommendations provided in the American College of Chest Physicians Guidelines13 include the use of low-molecular weight heparin (LMWH) upon confirmation of hemostasis (Grade 2B), combined use of IPC and LDUH (Grade 2C), combined use of IPC and ES in cases where anticoagulants are contraindicated (Grade 1C+), and treatment with LMWH or an oral-dose vitamin K antagonist during rehabilitation (Grade 1C). Christie et al.14 recommended treatment with LMWH within 72 h after injury or re-treatment with the same drug within 24 h after surgery. Further, no difference has been detected in the incidence of DVT or hemorrhagic complications between patients receiving 5000 U of unfractionated heparin every 8 h and those receiving 30 mg LMWH every 12 h, if treatment was started within 72 h after injury.15 We have no objection to the view that LMWH or LDUH has a central role in the prevention of DVT among patients with spinal cord injury, even in the patients treated surgically. However, there is a particular need to establish the use of these drugs during the acute stage of spinal cord injury.
Conclusion
-
1
DVT can develop at the very-acute stage of spinal cord injury.
-
2
The incidence of DVT increased with more severe paralysis.
-
3
Ultrasonography is a simple and valid means of detecting DVT.
-
4
Frequent ultrasonogtraphy during early stage is useful for detecting asymptomatic DVT in acute SCI patients.
Data archiving
There were no data to deposit.
References
Teasell RW, Hsieh JT, Aubut JA, Eng JJ, Krassioukov A, Tu L et al. Venous thromboembolism following spinal cord injury. Arch Phys Med Rehabil 2009; 90: 232–245.
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Furlan JC1, Fehlings MG . Cardiovascular complications after acute spinal cord injury: pathophysiology, diagnosis, and management. Neurosurg Focus 2008; 25: E13.
Miranda AR, Hassouna HI . Mechanisms of thrombosis in spinal cord injury. Hematol Oncol Clin North Am 2000; 14: 401–416.
Jones T, Ugalde V, Franks P, Zhou H, White RH . Venous thromboembolism after spinal cord injury: incidence, time course, and associated risk factors in 16,240 adults and children. Arch Phys Med Rehabil 2005; 86: 2240–2247.
Waring WP, Karunas RS . Acute spinal cord injuries and the incidence of clinically occurring. Paraplegia 1991; 29: 8–16.
Sugimoto Y, Ito Y, Tomioka M, Tanaka M, Hasegawa Y, Nakago K et al. Deep venous thrombosis in patients with acute cervical spinal cord injury in a Japanese population: assessment with Doppler ultrasonography. J Orthop Sci 2009; 14: 374–376.
Chen CJ, Wang CJ, Huang CC . The value of D-dimer in the detection of early deep-vein thrombosis after total knee arthroplasty in Asian patients: a cohort study. Thromb J 2008; 6: 5.
Shiota N, Sato T, Nishida K, Matsuo M, Takahara Y, Mitani S et al. Changes in LPIA D-dimer levels after total hip or knee arthroplasty relevant to deep-vein thrombosis diagnosed by bilateral ascending venography. J Orthop Sci 2002; 7: 444–450.
Mattos MA, Melendres G, Sumner DS, Hood DB, Barkmeier LD, Hodgson KJ et al. Prevalence and distribution of calf vein thrombosis in patients with symptomatic deep venous thrombosis: a color-flow duplex study. J Vasc Surg 1996; 24: 738–744.
Persson AV, Jones C, Zide R, Jewell ER . Use of the triplex scanner in diagnosis of deep venous thrombosis. Arch Surg 1989; 124: 593–596.
Comerota AJ, Katz ML, Greenwald LL, Leefmans E, Czeredarczuk M, White JV . Venous duplex imaging: should it replace hemodynamic tests for deep venous thrombosis? J Vasc Surg 1990; 11: 53–59.
Hirsh J, Guyatt G, Albers GW, Harrington R, Schünemann HJ . American College of Chest Physicians. Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133: 71S–109S.
Christie S, Thibault-Halman G, Casha S . Acute pharmacological DVT prophylaxis after spinal cord injury. J Neurotrauma 2011; 28: 1509–1514.
Spinal Cord Thromboprophylaxis Investigators. Prevention of venous thromboembolism in the acutetraumatic phase after spinal cord injury: a randamized, multicenter trial comparing low-dose heparin plus intermittent pneumatic compression with enoxaparin. J Trauma 2003; 54: 1116–1124 discussion 1125–1126.
Acknowledgements
We thank the sonographers in our hospital, Kiyoshi Saito, Mikiko Matsuzaki and Satoshi Yoshino for their effort.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Matsumoto, S., Suda, K., Iimoto, S. et al. Prospective study of deep vein thrombosis in patients with spinal cord injury not receiving anticoagulant therapy. Spinal Cord 53, 306–309 (2015). https://doi.org/10.1038/sc.2015.4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.4
This article is cited by
-
Risk factors of postoperative deep vein thrombosis (DVT) under low molecular weight heparin (LMWH) prophylaxis in patients with thoracolumbar fractures caused by high-energy injuries
Journal of Thrombosis and Thrombolysis (2021)
-
Rapidly progressive cervical myelopathy had a high risk of developing deep venous thrombosis: a prospective observational study in 289 cases with degenerative cervical spine disease
Spinal Cord (2019)