Abstract
Poor sleep is associated with the risk of developing chronic pain, but how sleep contributes to pain chronicity remains unclear. Here we show that following peripheral nerve injury, cholinergic neurons in the anterior nucleus basalis (aNB) of the basal forebrain are increasingly active during nonrapid eye movement (NREM) sleep in a mouse model of neuropathic pain. These neurons directly activate vasoactive intestinal polypeptide-expressing interneurons in the primary somatosensory cortex (S1), causing disinhibition of pyramidal neurons and allodynia. The hyperactivity of aNB neurons is caused by the increased inputs from the parabrachial nucleus (PB) driven by the injured peripheral afferents. Inhibition of this pathway during NREM sleep, but not wakefulness, corrects neuronal hyperactivation and alleviates pain. Our results reveal that the PB–aNB–S1 pathway during sleep is critical for the generation and maintenance of chronic pain. Inhibiting this pathway during the sleep phase could be important for treating neuropathic pain.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
All data are available in the main text or the supplementary materials. Source data are provided with this paper.
Code availability
The codes used in this study are open-source and accessible online.
References
Colloca, L. et al. Neuropathic pain. Nat. Rev. Dis. Prim. 3, 17002 (2017).
Campbell, J. N. & Meyer, R. A. Mechanisms of neuropathic pain. Neuron 52, 77–92 (2006).
Woolf, C. J. & Mannion, R. J. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet 353, 1959–1964 (1999).
Finan, P. H., Goodin, B. R. & Smith, M. T. The association of sleep and pain: an update and a path forward. J. Pain. 14, 1539–1552 (2013).
Haack, M., Simpson, N., Sethna, N., Kaur, S. & Mullington, J. Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology 45, 205–216 (2020).
Alexandre, C. et al. Decreased alertness due to sleep loss increases pain sensitivity in mice. Nat. Med. 23, 768–774 (2017).
Choy, E. H. The role of sleep in pain and fibromyalgia. Nat. Rev. Rheumatol. 11, 513–520 (2015).
Santello, M. & Nevian, T. Dysfunction of cortical dendritic integration in neuropathic pain reversed by serotoninergic neuromodulation. Neuron 86, 233–246 (2015).
Woolf, C. J. & Salter, M. W. Neuronal plasticity: increasing the gain in pain. Science 288, 1765–1769 (2000).
Kuner, R. & Flor, H. Structural plasticity and reorganisation in chronic pain. Nat. Rev. Neurosci. 18, 20–30 (2016).
Bliss, T. V., Collingridge, G. L., Kaang, B. K. & Zhuo, M. Synaptic plasticity in the anterior cingulate cortex in acute and chronic pain. Nat. Rev. Neurosci. 17, 485–496 (2016).
Huang, J. et al. A neuronal circuit for activating descending modulation of neuropathic pain. Nat. Neurosci. 22, 1659–1668 (2019).
Liu, Y. et al. Touch and tactile neuropathic pain sensitivity are set by corticospinal projections. Nature 561, 547–550 (2018).
Segerdahl, A. R., Mezue, M., Okell, T. W., Farrar, J. T. & Tracey, I. The dorsal posterior insula subserves a fundamental role in human pain. Nat. Neurosci. 18, 499–500 (2015).
Basbaum, A. I., Bautista, D. M., Scherrer, G. & Julius, D. Cellular and molecular mechanisms of pain. Cell 139, 267–284 (2009).
Hua, T. et al. General anesthetics activate a potent central pain-suppression circuit in the amygdala. Nat. Neurosci. 23, 854–868 (2020).
Eto, K. et al. Inter-regional contribution of enhanced activity of the primary somatosensory cortex to the anterior cingulate cortex accelerates chronic pain behavior. J. Neurosci. 31, 7631–7636 (2011).
Kim, S. K. & Nabekura, J. Rapid synaptic remodeling in the adult somatosensory cortex following peripheral nerve injury and its association with neuropathic pain. J. Neurosci. 31, 5477–5482 (2011).
Cichon, J., Blanck, T. J. J., Gan, W. B. & Yang, G. Activation of cortical somatostatin interneurons prevents the development of neuropathic pain. Nat. Neurosci. 20, 1122–1132 (2017).
Okada, T. et al. Pain induces stable, active microcircuits in the somatosensory cortex that provide a therapeutic target. Sci. Adv. 7, eabd8261 (2021).
Rolls, A. et al. Sleep to forget: interference of fear memories during sleep. Mol. Psychiatry 18, 1166–1170 (2013).
Aton, S. J. et al. Visual experience and subsequent sleep induce sequential plastic changes in putative inhibitory and excitatory cortical neurons. Proc. Natl Acad. Sci. USA 110, 3101–3106 (2013).
Aton, S. J. et al. Mechanisms of sleep-dependent consolidation of cortical plasticity. Neuron 61, 454–466 (2009).
Klinzing, J. G., Niethard, N. & Born, J. Mechanisms of systems memory consolidation during sleep. Nat. Neurosci. 22, 1598–1610 (2019).
Euston, D. R., Tatsuno, M. & McNaughton, B. L. Fast-forward playback of recent memory sequences in prefrontal cortex during sleep. Science 318, 1147–1150 (2007).
Li, W., Ma, L., Yang, G. & Gan, W. B. REM sleep selectively prunes and maintains new synapses in development and learning. Nat. Neurosci. 20, 427–437 (2017).
Yang, G. et al. Sleep promotes branch-specific formation of dendritic spines after learning. Science 344, 1173–1178 (2014).
Frank, M. G., Issa, N. P. & Stryker, M. P. Sleep enhances plasticity in the developing visual cortex. Neuron 30, 275–287 (2001).
Chauvette, S., Seigneur, J. & Timofeev, I. Sleep oscillations in the thalamocortical system induce long-term neuronal plasticity. Neuron 75, 1105–1113 (2012).
Pfeffer, C. K., Xue, M., He, M., Huang, Z. J. & Scanziani, M. Inhibition of inhibition in visual cortex: the logic of connections between molecularly distinct interneurons. Nat. Neurosci. 16, 1068–1076 (2013).
Pi, H. J. et al. Cortical interneurons that specialize in disinhibitory control. Nature 503, 521–524 (2013).
Magnus, C. J. et al. Ultrapotent chemogenetics for research and potential clinical applications. Science 364, eaav5282 (2019).
Gradinaru, V. et al. Molecular and cellular approaches for diversifying and extending optogenetics. Cell 141, 154–165 (2010).
Alitto, H. J. & Dan, Y. Cell-type-specific modulation of neocortical activity by basal forebrain input. Front. Syst. Neurosci. 6, 79 (2012).
Letzkus, J. J. et al. A disinhibitory microcircuit for associative fear learning in the auditory cortex. Nature 480, 331–335 (2011).
Askew, C.E., Lopez, A.J., Wood, M.A. & Metherate, R. Nicotine excites VIP interneurons to disinhibit pyramidal neurons in auditory cortex. Synapse 73, e22116 (2019).
Zaborszky, L. et al. Specific basal forebrain-cortical cholinergic circuits coordinate cognitive operations. J. Neurosci. 38, 9446–9458 (2018).
Fu, Y. et al. A cortical circuit for gain control by behavioral state. Cell 156, 1139–1152 (2014).
Kim, J. H. et al. Selectivity of neuromodulatory projections from the basal forebrain and locus ceruleus to primary sensory cortices. J. Neurosci. 36, 5314–5327 (2016).
Wall, N. R. et al. Brain-wide maps of synaptic input to cortical interneurons. J. Neurosci. 36, 4000–4009 (2016).
Zingg, B. et al. AAV-mediated anterograde transsynaptic tagging: mapping corticocollicular input-defined neural pathways for defense behaviors. Neuron 93, 33–47 (2017).
Broussard, G. J. et al. In vivo measurement of afferent activity with axon-specific calcium imaging. Nat. Neurosci. 21, 1272–1280 (2018).
Borden, P. M. et al. A fast genetically encoded fluorescent sensor for faithful in vivo acetylcholine detection in mice, fish, worms and flies. BioRxiv, https://doi.org/10.1101/2020.02.07.939504 (2020).
Ballinger, E. C., Ananth, M., Talmage, D. A. & Role, L. W. Basal forebrain cholinergic circuits and signaling in cognition and cognitive decline. Neuron 91, 1199–1218 (2016).
Peng, C. et al. Gene editing vectors for studying nicotinic acetylcholine receptors in cholinergic transmission. Eur. J. Neurosci. 50, 2224–2238 (2019).
Saunders, A. et al. A direct GABAergic output from the basal ganglia to frontal cortex. Nature 521, 85–89 (2015).
Hunker, A. C. et al. Conditional single vector CRISPR/SaCas9 viruses for efficient mutagenesis in the adult mouse nervous system. Cell Rep. 30, 4303–4316 (2020).
Tervo, D. G. et al. A designer AAV variant permits efficient retrograde access to projection neurons. Neuron 92, 372–382 (2016).
Huang, L. et al. BDNF produced by cerebral microglia promotes cortical plasticity and pain hypersensitivity after peripheral nerve injury. PLoS Biol. 19, e3001337 (2021).
Saper, C. B. & Loewy, A. D. Efferent connections of the parabrachial nucleus in the rat. Brain Res. 197, 291–317 (1980).
Hu, R., Jin, S., He, X., Xu, F. & Hu, J. Whole-brain monosynaptic afferent inputs to basal forebrain cholinergic system. Front Neuroanat. 10, 98 (2016).
Chiang, M. C. et al. Parabrachial complex: a hub for pain and aversion. J. Neurosci. 39, 8225–8230 (2019).
Huang, T. et al. Identifying the pathways required for coping behaviours associated with sustained pain. Nature 565, 86–90 (2019).
Kaur, S. & Saper, C. B. Neural circuitry underlying waking up to hypercapnia. Front Neurosci. 13, 401 (2019).
Chen, C. et al. Long-term imaging of dorsal root ganglia in awake behaving mice. Nat. Commun. 10, 3087 (2019).
Jones, B. E. Activity, modulation and role of basal forebrain cholinergic neurons innervating the cerebral cortex. Prog. Brain Res. 145, 157–169 (2004).
Lee, M. G., Hassani, O. K., Alonso, A. & Jones, B. E. Cholinergic basal forebrain neurons burst with theta during waking and paradoxical sleep. J. Neurosci. 25, 4365–4369 (2005).
Xu, M. et al. Basal forebrain circuit for sleep-wake control. Nat. Neurosci. 18, 1641–1647 (2015).
Fuller, P. M., Sherman, D., Pedersen, N. P., Saper, C. B. & Lu, J. Reassessment of the structural basis of the ascending arousal system. J. Comp. Neurol. 519, 933–956 (2011).
Qiu, M. H., Chen, M. C., Fuller, P. M. & Lu, J. Stimulation of the pontine parabrachial nucleus promotes wakefulness via extra-thalamic forebrain circuit nodes. Curr. Biol. 26, 2301–2312 (2016).
Kaur, S. et al. Glutamatergic signaling from the parabrachial nucleus plays a critical role in hypercapnic arousal. J. Neurosci. 33, 7627–7640 (2013).
Irmak, S. O. & de Lecea, L. Basal forebrain cholinergic modulation of sleep transitions. Sleep 37, 1941–1951 (2014).
Bjurstrom, M. F. & Irwin, M. R. Polysomnographic characteristics in nonmalignant chronic pain populations: a review of controlled studies. Sleep Med. Rev. 26, 74–86 (2016).
Ito, H. et al. Chronic pain recruits hypothalamic dynorphin/kappa opioid receptor signalling to promote wakefulness and vigilance. Brain 00, 1–14 (2022).
Krettek, J. E. & Price, J. L. Amygdaloid projections to subcortical structures within the basal forebrain and brainstem in the rat and cat. J. Comp. Neurol. 178, 225–253 (1978).
Stickgold, R. Sleep-dependent memory consolidation. Nature 437, 1272–1278 (2005).
Cichon, J. et al. Imaging neuronal activity in the central and peripheral nervous systems using new Thy1.2-GCaMP6 transgenic mouse lines. J. Neurosci. Methods 334, 108535 (2020).
Taniguchi, H. et al. A resource of Cre driver lines for genetic targeting of GABAergic neurons in cerebral cortex. Neuron 71, 995–1013 (2011).
He, M. et al. Strategies and tools for combinatorial targeting of GABAergic neurons in mouse cerebral cortex. Neuron 91, 1228–1243 (2016).
Madisen, L. et al. A robust and high-throughput Cre reporting and characterization system for the whole mouse brain. Nat. Neurosci. 13, 133–140 (2010).
Rossi, J. et al. Melanocortin-4 receptors expressed by cholinergic neurons regulate energy balance and glucose homeostasis. Cell Metab. 13, 195–204 (2011).
Vong, L. et al. Leptin action on GABAergic neurons prevents obesity and reduces inhibitory tone to POMC neurons. Neuron 71, 142–154 (2011).
Platt, R. J. et al. CRISPR-Cas9 knockin mice for genome editing and cancer modeling. Cell 159, 440–455 (2014).
Cichon, J., Sun, L. & Yang, G. Spared nerve injury model of neuropathic pain in Mice. Bio Protoc. 8, e2777 (2018).
Yang, G., Pan, F., Chang, P. C., Gooden, F. & Gan, W. B. Transcranial two-photon imaging of synaptic structures in the cortex of awake head-restrained mice. Methods Mol. Biol. 1010, 35–43 (2013).
Giovannucci, A. et al. CaImAn an open source tool for scalable calcium imaging data analysis. eLife 8, e38173 (2019).
Pnevmatikakis, E. A. & Giovannucci, A. NoRMCorre: an online algorithm for piecewise rigid motion correction of calcium imaging data. J. Neurosci. Methods 291, 83–94 (2017).
Pnevmatikakis, E. A. et al. Simultaneous denoising, deconvolution, and demixing of calcium imaging data. Neuron 89, 285–299 (2016).
Vogelstein, J. T. et al. Fast nonnegative deconvolution for spike train inference from population calcium imaging. J. Neurophysiol. 104, 3691–3704 (2010).
Yang, G., Pan, F. & Gan, W. B. Stably maintained dendritic spines are associated with lifelong memories. Nature 462, 920–924 (2009).
Yang, G., Pan, F., Parkhurst, C. N., Grutzendler, J. & Gan, W. B. Thinned-skull cranial window technique for long-term imaging of the cortex in live mice. Nat. Protoc. 5, 201–208 (2010).
Urban, D. J. & Roth, B. L. DREADDs (designer receptors exclusively activated by designer drugs): chemogenetic tools with therapeutic utility. Annu. Rev. Pharmacol. Toxicol. 55, 399–417 (2015).
Dixon, W. J. Efficient analysis of experimental observations. Annu. Rev. Pharmacol. Toxicol. 20, 441–462 (1980).
Chaplan, S. R., Bach, F. W., Pogrel, J. W., Chung, J. M. & Yaksh, T. L. Quantitative assessment of tactile allodynia in the rat paw. J. Neurosci. Methods 53, 55–63 (1994).
Cheng, L. et al. Identification of spinal circuits involved in touch-evoked dynamic mechanical pain. Nat. Neurosci. 20, 804–814 (2017).
Li, M., Zhou, H., Teng, S. & Yang, G. Activation of VIP interneurons in the prefrontal cortex ameliorates neuropathic pain aversiveness. Cell Rep. 40, 111333 (2022).
Sun, L. et al. Targeted ubiquitination of sensory neuron calcium channels reduces the development of neuropathic pain. Proc. Natl Acad. Sci. USA 119, e2118129119 (2022).
Acknowledgements
We thank W. Gan (New York University) for providing Thy1-GCaMP6s mice, L. Looger (Janelia Research Campus) for providing the iAChSnFR sensor, R. Drenan (Wake Forest University) for providing AAVs encoding Chrnb2 and Chrna7 sgRNA sequences and Yang Lab members for helpful discussion. This work was supported by National Institutes of Health grants R01AA027108 (to G.Y.), R35GM131765 (to G.Y.) and the Columbia University Medical Center Target of Opportunity award (to G.Y.).
Author information
Authors and Affiliations
Contributions
H.Z. and G.Y. conceived the project and designed the experiments. H.Z. and R.Z. performed Ca2+ imaging and EEG/EMG recordings. H.Z. and M.L. performed optogenetic manipulation and spine imaging. H.Z. and L.S. performed DRG imaging. H.Z. performed all the other experiments. H.Z., M.L. and R.Z. analyzed the data. All authors contributed to data interpretation. H.Z. and G.Y. wrote the manuscript with input from all authors.
Corresponding author
Ethics declarations
Competing interests
All the authors declare no competing interests.
Peer review
Peer review information
Nature Neuroscience thanks Rohini Kuner, Patrick Sheets and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Alterations in S1 inhibitory neuronal Ca2+ activity are reduced by silencing VIP INs during sleep after SNI.
a, Schematic of S1 local circuitry. b, SNI-induced changes in neuronal Ca2+ activity (mean ± s.e.m.) in S1 of resting awake mice (n = 192, 93, 100, and 86 cells from three mice per group). PNs, P = 0.23 (day 1), 0.0026 (day 3), < 0.0001 (day 5–30); VIP, P = 0.017 (day 1), < 0.0001 (day 2–7), 0.0046, 0.0036; SST, P = 0.46, 0.68, 0.53, 0.034, 0.0043, 0.018, 0.014; PV, P = 0.083, 0.0006, < 0.0001 (day 5, 7), 0.004, 0.023, 0.007. c, Top, experimental design for chemogenetic inhibition of S1 VIP INs via hM4D(Gi) and Ca2+ imaging of VIP and SST INs. Bottom, representative two-photon images of GCaMP/mCherry-expressing VIP INs (arrows) and GCaMP-expressing SST INs (bottom; 4 mice). d, Average Ca2+ traces (mean with 95% CI) of VIP and SST INs before and 1 h after CNO injection (n = 168 and 226 cells from four mice). Acute inhibition of VIP INs (****P < 0.0001) increases SST neuron activity (****P < 0.0001) in SNI mice. e, Daily inhibition of VIP INs at ZT2 reduces SNI-induced SST hypoactivity (n = 217, 177, 190 cells from four mice per group; ****P < 0.0001). f, Top, experimental design for chemogenetic inhibition of S1 VIP INs via PSAM4-GlyR and Ca2+ imaging of PV INs. Bottom, two-photon images of EGFP-expressing VIP INs and GCaMP-expressing PV INs (13 mice). g, Similar to (d), but for PV INs before and after uPSEM817 injection (n = 203 cells from four mice; ****P < 0.0001). h, Similar to (e), but for PV INs after VIP inhibition (n = 142, 116, 148 cells from three mice per group; ****P < 0.0001). Box bounds and center, quartiles and median; whiskers, min and max (d, e, g, h). *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001 by two-sided Wilcoxon (b, d, g) or Kolmogorov-Smirnov test (e, h). Detailed statistics are in Supplementary Table 1.
Extended Data Fig. 2 Silencing S1 VIP INs during sleep prevents persistent ongoing pain after SNI.
a, Schematic of experimental timeline and the conditioned place preference (CPP) test. Two weeks after viral infection, mice were subjected to SNI and daily inhibition of the target cells in the sleep or wake phase for 5 days. CPP tests were performed 2–3 weeks after the last inhibition session. b, Representative heat maps showing time spent in CPP chambers. c, Time spent in the saline- and lidocaine-paired chambers for individual mice (n = 5, 5, 5, 6 mice; saline vs. lidocaine, P = 0.87, 0.0004, 0.0001, 0.90; related to Fig. 2d). d, Time spent in the saline- and lidocaine-paired chambers for individual mice (n = 6, 6, 6, 5, 5, 4 mice; saline vs. lidocaine, P = 0.81, 0.0035, 0.0063, 0.18, 0.74, 0.058; related to Fig. 2f). e, Time spent in the saline- and lidocaine-paired chambers for individual mice (n = 5 mice per group, saline vs. lidocaine, P = 0.91, 0.0022, 0.019, 0.66; related to Fig. 5e). f, Time spent in the saline- and lidocaine-paired chambers for individual mice (n = 4, 5, 4, 5 mice; saline vs. lidocaine, P = 0.36, 0.012, 0.011, 0.12; related to Fig. 6e). g, Time spent in the saline- and lidocaine-paired chambers for individual mice (n = 6 mice per group; saline vs. lidocaine, P = 0.11, 0.0010, 0.97, 0.49; related to Fig. 7b). Inset, experimental timeline. Mean ± s.e.m. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; NS, not significant; by two-sided paired t-test. Detailed statistics are in Supplementary Table 1.
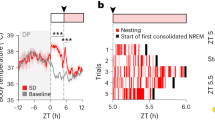
Extended Data Fig. 3 The sleep-wake structure and EEG power analysis in mice with or without neuropathic pain.
a, Mean NREM sleep distribution (n = 5 mice per group). No difference in sleep pattern following 3- or 7-day acclimation (F(7, 64) = 0.98, P = 0.45). The VIP-Cre transgene has no effect on sleep pattern (F(7, 64) = 0.26, P = 0.97 vs. C57 3-day acclimation). b, Percentages of time in wake, NREM and REM sleep during the rest and active phase of the mouse (n = 5 mice). c, EEG analysis for naïve VipIRES-Cre mice expressing eNpHR (no surgery) (n = 4 mice per group). Experimental timeline for optogenetic inhibition (left), mean EEG power density (right) and percentages of time (inset) in wake, NREM and REM sleep. VIP inhibition has no effect on EEG power intensity in wake (P = 0.68), NREM (P = 0.55) and REM (P = 0.89) sleep. d, EEG analysis for VipIRES-Cre mice expressing EYFP (n = 5 mice; related to Fig. 2f). Mean EEG power density in NREM (left) and quantification (right) before, 3 and 14 days after SNI. Inset, percentages of wake, NREM, and REM. SNI decreases the power of δ wave (P = 0.0020, 0.24 vs. Pre) and increases the power of α (P = 0.014, 0.0050) and σ waves (P = 0.016, 0.017) in NREM sleep. e, Similar to (d), but for VipIRES-Cre mice expressing eNpHR (n = 10 mice; related to Fig. 2f). Daily inhibition of VIP INs reverses alterations in NREM power density after SNI (δ, P = 0.033, 0.61; θ, 0.27, 0.20; α, 0.0001, 0.86; σ, 0.0017, 0.60 vs. Pre). Mean ± s.e.m. Shading in a, c, d, e, 95% CI. *P < 0.05, **P < 0.01, ***P < 0.001; NS, not significant; by two-sided two-way ANOVA (a), Mann-Whitney (c) or paired t-test (d, e). Detailed statistics are in Supplementary Table 1.
Extended Data Fig. 4 Pharmacological inhibition of α7-containing nAChRs or mAChRs in S1 has little effect on SNI-induced allodynia in mice.
a, Left, schematic of experimental design to evaluate intracortical drug spread with Alexa633 hydrazide (0.15 µl, 1 µM). Confocal images of serial brain slices (middle) and quantification (right) showing Alexa633 fluorescence mainly restricted in L2/3 of S1 (n = 3 mice). L, lateral; ML, midline; D, dorsal; V, ventral. a.u., arbitrary units. b–d, Left, schematic of experimental design. Mice received daily intracortical (i.c.) injections of AChR antagonist (0.15 µl), at either ZT2 or ZT14, from days 1 to 5 after SNI. Control mice received vehicle (ACSF) injections. Right, nociceptive thresholds in mice. Vehicle controls (dashed line) were shared between (b–d) and Fig. 4d. b, Administration of methyllycaconitine (MLA, 10 nM), an antagonist of α7-containing nAChRs, at ZT2 has minor effects on alleviating SNI-induced mechanical allodynia in mice (n = 6 mice in ZT2 group tested for punctate pain; n = 5 mice per group for other tests; SNI-ZT2 vs. SNI, punctate, F(9, 90) = 2.50, P = 0.013; dynamic, F(3, 27) = 8.83, P = 0.0002; cold, F(3, 27) = 0.65, P = 0.59; hot, F(3, 27) = 0.49, P = 0.69). c, Administration of scopolamine (20 µM), a pan-mAChR antagonist, has no effects on alleviating SNI-induced allodynia in mice (n = 6 mice per group; SNI-ZT2 vs. SNI, punctate, F(9, 90) = 1.49, P = 0.16; dynamic, F(3, 30) = 0.50, P = 0.69; cold, F(3, 30) = 0.07, P = 0.97; hot, F(3, 30) = 0.78, P = 0.51). d, Administration of AF-DX 116 (150 nM) and PD102807 (200 nM), M2- and M4-containing mAChR antagonists, has no effects on alleviating SNI-induced allodynia in mice (n = 5 mice per group; SNI-ZT2 vs. SNI, punctate, F(9, 81) = 1.99, P = 0.051; dynamic, F(3, 27) = 1.07, P = 0.38; cold, F(3, 27) = 0.95, P = 0.43; hot, F(3, 27) = 1.63, P = 0.21). Mean ± s.e.m. *P < 0.05, ** P < 0.01, *** P < 0.001; NS, not significant; by two-way ANOVA followed by Bonferroni’s test (two-sided). Detailed statistics are in Supplementary Table 1.
Extended Data Fig. 5 Neuronal and behavioral effects of CRISPR/Cas9-mediated cell-type specific Chrnb2 and/or Chrna7 deletion in S1.
a, Experimental design for selective knockout (KO) of Chrnb2 (β2) or Chrna7 (α7) in S1 VIP INs and expression of hM3D(Gq) in aNB→S1 projections (left), two-photon images of VIP INs expressing GCaMP6s and Cas9-mCherry (middle), and Ca2+ activity before and 20 min post-CNO (right). VIP INs increase activity upon activation of aNB→S1 projections, which is abolished with β2 KO. (non-KO/KO cells/mice; n = 53/117/three, 73/96/four, 61/106/four; KO vs. non-KO, P = 0.87, 0.0054, 0.23). b, Experimental design for β2 or α7 KO in VIP (left), images of Cas9-EGFP+ VIP and GCaMP6s+ PNs (middle), and PN Ca2+ activity before and after SNI (n = 208, 253, 253, 189 cells from three mice per group). SNI-induced PN hyperactivation is abolished after VIP β2 KO (D14, wake, F(2, 1458) = 6.91, P = 0.0005; NREM, F(2, 1458) = 6.91, P < 0.0001). c, VIP β2 or α7 KO has no effects on baseline nociceptive thresholds (n = 11, 5, 5 mice; punctate, P = 0.17, 0.40, 0.78). d, VIP α7 KO partially reduces SNI-induced allodynia (n = 6, 5, 5 mice; punctate, P = 0.24, 0.44, 0.017; dynamic, 0.035, 0.031, 0.0087; cold, 0.015, 0.10, 0.067; hot, 0.042, 0.27, 0.20). e,f,g, Experimental design for β2 and/or α7 KO in SST, PV, or PNs in S1 (e), which has no effects on baseline nociceptive thresholds (f; n = 9, 9, 5, 5, 4, 4, 5 mice; punctate, P = 0.99, 0.13, 0.37, 0.75, 0.43, 0.83, 0.25), and SNI-induced allodynia (g; n = 9, 9, 5, 5, 4, 4, 5 mice; SST-α7 KO, punctate, F(8, 96) = 0.09, P = 0.99; dynamic, F(3, 36) = 0.79, P = 0.51; cold, F(3, 36) = 0.02, P = 0.99; hot, F(3, 36) = 0.31, P = 0.81). Mean ± s.e.m. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; NS, not significant; by two-sided Wilcoxon (a, c, f), Kolmogorov-Smirnov (a), two-way ANOVA followed by Bonferroni’s test (vs. SNI; b, d, g). Detailed statistics are in Supplementary Table 1.
Extended Data Fig. 6 Characterization of aNB→S1 projections co-releasing ACh/GABA and their role in neuropathic pain.
a, Schematic of experimental design. Retrobeads were injected into L1–L2/3 of S1 to trace S1-projecting cells in the aNB region (3 mice). b,c, Immunofluorescence images in the aNB region showing ChAT+ cells (b) and colocalization of ChAT, GAD2, and Retrobeads (c). d, Quantification of data shown in (c) (3 mice). Percentages of ChAT+ cells expressing GAD2, S1-projecting (Retrobeads+) cells expressing ChAT, or both ChAT and GAD2. e, Left, experimental design and timeline for CRISPR/Cas9-mediated deletion of Slc32a1 gene (encoding VGAT) in aNB cholinergic neurons and labeling of their axonal boutons with synaptophysin (Syp)-mRuby. Middle, immunofluorescence images showing colocalization of VGAT and VAChT in Syp-mRuby+ cholinergic boutons in S1. Right, percentages of VAChT+ boutons expressing VGAT in control and Slc32a1 knockout (KO) mice (n = 4 mice per group). Arrows, Syp-mRuby+ boutons. Scramble, a control vector without Slc32a1 sgRNA sequence. f, Left, experimental design for selective deletion of Slc32a1 gene in aNB–S1 projection neurons. Right, nociceptive thresholds under various conditions (n = 6, 5, 6 mice). VGAT KO in aNB–S1 projection neurons has no marked effects on SNI-induced mechanical and thermal allodynia in mice (punctate, P = 0.067, 0.081, 0.057; dynamic, 0.068, 0.19, 0.0093; cold, 0.089, 0.99, 0.82; hot, 0.058, 0.048, 0.16). Mean ± s.e.m. *P < 0.05, **P < 0.01; NS, not significant; by two-sided Mann-Whitney U test (e) or two-way ANOVA followed by Bonferroni’s test (f). See detailed statistics are in Supplementary Table 1.
Extended Data Fig. 7 Retrograde labeling of aNB-projecting neurons in the midbrain.
a, Schematic of experimental design. Retrobeads were injected into the aNB to retrogradely label the aNB-projecting neurons in PB of ChATIRES-Cre or Slc17a6IRES-Cre mice. ChAT+ or vGLUT2+ PB neurons were labeled by AAVs encoding Cre-inducible EGFP. b, Images showing red Retrobeads injected into the aNB region (AP -0.8 – -1.1 mm) (repeated in 3 mice). c–f, Coronal brain sections showing the distribution of Retrobeads in the midbrain 10 days after injection (3 mice). g, h, Percentages of aNB-projecting neurons in midbrain nuclei at AP -4.6 – -4.9 mm (g) and -5.1 – -5.4 mm (h) (n = 3 mice). Inset: fraction of Retrobeads+ cells in the lateral PB (lPB) and the medial PB (mPB) ipsilateral or contralateral to the injection site. i, Colocalization of Retrobeads+ somas and NeuN+ nuclei in PB. Arrows indicate Retrobeads+NeuN+ cells. j, Percentages of NeuN+ cells containing Retrobeads (3 mice). k, Colocalization of Retrobeads+, EGFP-labeled vGLUT2+, and ChAT immunoreactive somas in PB of Slc17a6IRES-Cre mice. Yellow and magenta arrows indicate vGLUT2+Retrobeads+ and ChAT+Retrobeads+ cells, respectively (3 mice). l, Percentages of Retrobeads+ cells expressing vGLUT2 and/or ChAT in lPB and mPB (n = 3 mice). m, Confocal images of coronal sections from ChATIRES-Cre mice. Upper, colocalization of Retrobeads+ and calcitonin gene-related peptide immunoreactive (CGRP+) somas in the external lPB (elPB) and the external mPB (emPB) (3 mice). Red and white arrows indicate Retrobeads+ and CGRP+ cells, respectively. Lower, colocalization of Retrobeads+, EGFP-labeled ChAT+, and CGRP+ somas in mPB (2 mice). Yellow, white, and magenta arrows indicate Retrobeads+ChAT+CGRP–, Retrobeads+ChAT–CGRP–, and Retrobeads–ChAT–CGRP+ cells, respectively. n, Percentages of Retrobeads+ cells expressing CGRP in mPB and lPB (2 mice). Mean ± s.e.m.
Extended Data Fig. 8 A group of basal forebrain cholinergic neurons receive monosynaptic inputs from PB and preferentially project to the superficial layers of S1.
a, Schematic of experimental design to label PB→aNB→S1 projections. AAV1 encoding neuron-specific Cre recombinase was injected into PB. AAVs encoding Cre-inducible EGFP were injected into aNB to visualize neurons receiving monosynaptic inputs from PB. The distribution of EGFP+ axons across layers of S1 was examined. b, EGFP fluorescence superimposed on the light field images of the aNB region at various AP coordinates (3 mice). c, High-magnitude images of the aNB region at various AP coordinates, stained for DAPI. Arrows indicate EGFP+ cells receiving monosynaptic inputs from PB. d, Distribution of basal forebrain cells receiving monosynaptic inputs from PB (n = 3 mice). e, Immunofluorescence coronal sections of the basal forebrain showing the colocalization of EGFP+ and ChAT immunoreactive (ChAT+) cells (3 mice). Blue dashed lines profile the empirical region of NB with the hallmark of magnocellular neurons. f, Left, representative images of aNB at different AP coordinates showing the heterogenous distribution of ChAT+ cells receiving monosynaptic inputs from PB (3 mice). Right, percentages of aNB ChAT+ cells receiving monosynaptic inputs from PB, in the rostral (AP -0.45 – -0.80 mm) and caudal (AP -0.80 – -1.15 mm) regions. g, Intensity distribution of EGFP+ axons (derived from aNB neurons receiving PB projections) across layers of S1 (n = 3 mice) compared with the distribution of projections from aNB ChAT+ cells (black line, from Supplementary Fig. 4; n = 4 mice). Mean ± s.e.m. L, lateral; ML, midline; D, dorsal; V, ventral; ic, internal capsule; GPe, external globus pallidus; GPi, internal globus pallidus; SI, substantia innominate.
Extended Data Fig. 9 Silencing PB→aNB projections during sleep reduces aNB→S1 projection hyperactivity and allodynia after SNI.
a-c, Schematic of experimental design for optogenetic inhibition of PB→aNB terminals (a), its acute effects on aNB axonal Ca2+ in S1 (b; solid lines, mean changes in Ca2+ signals; shading, 95% CI), and quantification of peak Ca2+ activity immediately following light stimulation (c; n = 137 boutons from three mice; wake, P = 0.84, 0.036, 0.0004; NREM, P = 0.033, 0.0003, < 0.0001). d, Schematic of viral injections for chemogenetic inhibition of PB→aNB projection cells and Ca2+ imaging in aNB→S1 axons of the aNB cells receiving PB projections. e, Within 1–1.5 h after uPSEM817 administration (0.3 mg kg−1; i.p. at ZT4) to inhibit PB→aNB projection cells, axonal Ca2+ in aNB→S1 projections was decreased more in NREM than in wake (n = 250 boutons from five mice; P < 0.0001). f, Daily inhibition of PB→aNB projection cells at ZT2 for 5 days following SNI effectively reduces aNB→S1 axonal Ca2+ activity on day 14 (n = 147, 161, 143, 159 boutons from three mice; SNI-ZT2 vs. SNI, P = 0.0005 wake, < 0.0001 NREM). g, Daily inhibition of PB→aNB projections at ZT2 for 5 days following SNI, reduces punctate (P = 0.0018, 0.0002, 0.0007), dynamic (P = 0.0005, < 0.0001, < 0.0001), cold (P = 0.013, 0.0002, 0.0014), and hot (P = 0.0050, 0.0007, 0.0009) allodynia 14, 21 and 28 days after SNI mice (n = 5 mice per group). IR: infrared radiant. Mean ± s.e.m. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; NS, not significant; by two-sided paired t (c), Wilcoxon (e), Kolmogorov-Smirnov (f) or two-way ANOVA followed by Bonferroni’s test (g). Detailed statistics are in Supplementary Table 1.
Extended Data Fig. 10 Inhibition of PB→aNB→S1 circuits during sleep reduces sleep fragmentation in SNI mice.
a–c, Number of wake (a), NREM (b), REM (c) episodes per hour. EEG/EMG recordings were performed during ZT2–ZT10. SNI increases the number of wake/NREM/REM episodes in the rest phase of the mouse (indicative of sleep fragmentation), which is mitigated after opto- or chemogenetic inhibition of PB–aNB–S1 circuits (n = 12, 11, 13, 5, 5, 5, 5, 10, 10 mice). Treatment I–IV vs. D14, P = 0.0019 (wake), < 0.0001 (NREM), 0.0002 (REM); Treatment V vs. D34, P = 0.0007 (wake), 0.0007 (NREM), 0.0001 (REM). d–h, Number of transitions between brain states per hour. EEG/EMG recordings were performed during ZT2–ZT10. SNI increases the number of transitions between brain states in the rest phase of the mouse, which is mitigated after opto- or chemogenetic inhibition of PB–aNB–S1 circuits (n = 12, 11, 13, 5, 5, 5, 5, 10, 10 mice). Treatment I–IV vs. D14, P = 0.0025 (wake→NREM), 0.0057 (NREM→wake), 0.0002 (NREM→REM), 0.0003 (REM→NREM), 0.0012 (REM→wake); treatment V vs. D34, P = 0.0007 (wake→NREM), 0.043 (NREM→wake), 0.0001 (NREM→REM), 0.81 (REM→NREM), < 0.0001 (REM→wake). Mice in treatment groups I–V are the same mice shown in Figs. 2f, 5e, 6e, and 7b. Pie graphs indicate the fraction of mice with (> 1× s.d.) or without (< 1× s.d.) changes in sleep compared to pre-SNI, where 1× s.d. is an arbitrary threshold. Mean ± s.e.m. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; NS, not significant; by two-sided Mann-Whitney U test. Gray symbols, vs. pre-SNI. Black symbols, vs. D14 or D34 post-SNI. Detailed statistics are in Supplementary Table 1.
Supplementary information
Supplementary Information
Supplementary Figs. 1–5.
Supplementary Data
Supporting data for Supplementary Figs. 1–5
Supplementary Table 1
Statistical details for Figs. 1–7, Extended Data Figs. 1–10 and Supplementary Figs. 1–5.
Supplementary Table 2
Mouse sex information for all experiments.
Source data
Source Data Fig. 1
Statistical source data for Fig. 1.
Source Data Fig. 2
Statistical source data for Fig. 2.
Source Data Fig. 3
Statistical source data for Fig. 3.
Source Data Fig. 4
Statistical source data for Fig. 4.
Source Data Fig. 5
Statistical source data for Fig. 5.
Source Data Fig. 6
Statistical source data for Fig. 6.
Source Data Fig. 7
Statistical source data for Fig. 7.
Source Data Extended Data Fig. 1
Statistical source data for Extended Data Fig. 1.
Source Data Extended Data Fig. 2
Statistical source data for Extended Data Fig. 2.
Source Data Extended Data Fig. 3
Statistical source data for Extended Data Fig. 3.
Source Data Extended Data Fig. 4
Statistical source data for Extended Data Fig. 4.
Source Data Extended Data Fig. 5
Statistical source data for Extended Data Fig. 5.
Source Data Extended Data Fig. 6
Statistical source data for Extended Data Fig. 6.
Source Data Extended Data Fig. 7
Statistical source data for Extended Data Fig. 7.
Source Data Extended Data Fig. 8
Statistical source data for Extended Data Fig. 8.
Source Data Extended Data Fig. 9
Statistical source data for Extended Data Fig. 9.
Source Data Extended Data Fig. 10
Statistical source data for Extended Data Fig. 10.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, H., Li, M., Zhao, R. et al. A sleep-active basalocortical pathway crucial for generation and maintenance of chronic pain. Nat Neurosci 26, 458–469 (2023). https://doi.org/10.1038/s41593-022-01250-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41593-022-01250-y