Abstract
Atrial fibrillation may affect blood pressure measurements. The ankle–brachial index (ABI) is a ratio of systolic blood pressure measured on the lower and upper limbs that may also be affected by arrhythmia. The purpose of the study was to investigate whether atrial fibrillation influenced ABI results. Ninety-nine patients (age 66.6±11 years, 63 males and 36 females) who underwent electrical cardioversion of atrial fibrillation were investigated. ABI measurements using the Doppler method were performed on both lower extremities before and after electrical cardioversion. Measurements were repeated three times and then averaged. The ABI using both lower limbs was lower before electrical cardioversion than after restoration to sinus rhythm (right side: 1.132 (1.065–1.210) during atrial fibrillation vs. 1.179 (1.080–1.242) in sinus rhythm, P=0.019; left side: 1.142 (1.075–1.222) during atrial fibrillation vs. 1.170 (1.098–1.255) in sinus rhythm, P=0.011). However, the upper 95% confidence interval (CI) margins for the median differences in ABI were 0.045 and 0.040 for right and left, respectively, suggesting that the observed difference was clinically insignificant. There was a significant correlation between measurements obtained before and after electrical cardioversion on both lower limbs (r=0.61, P<0.001 and r=0.67, P<0.001). The Bland–Altman plot showed good agreement between measurements performed using the Doppler method during atrial fibrillation and sinus rhythm. Study results showed that atrial fibrillation did not have a clinically important effect on ABI measurements.
Similar content being viewed by others
Introduction
The ankle–brachial index (ABI) is the ratio of the systolic blood pressure (SBP) measured at the ankle to SBP measured at the brachial artery.1, 2 The ABI is used for noninvasive diagnosis of occlusive peripheral artery disease (PAD), as an indicator of atherosclerosis and as a marker of cardiovascular disease.3, 4, 5 The threshold ABI value most commonly used is ⩽0.90 based on studies reporting >90% sensitivity and specificity to detect PAD compared with angiography.1, 2 Many factors may influence ABI measurement results, including the method of measurement, repeated measurements, height, sex, race and heart rate.6 During atrial fibrillation, blood pressure measurements and ABI calculations may be biased by high beat-to-beat variability of heart rate and stroke volume.7 Significant inter- and intra-observer errors during blood pressure measurements in subjects with atrial fibrillation have been documented and no accepted guidelines exist on how to perform blood pressure measurements during atrial fibrillation.8 Furthermore, there is no recommendation and few reports on how to measure ABI during atrial fibrillation. In daily practice, it is not routine to perform electrocardiogram recording or to analyze a patient’s cardiovascular history before ABI measurement. Thus, patients may have atrial fibrillation during ABI measurements.
The standard ABI measurement method is the Doppler method. Although it requires training, ABI results obtained using the Doppler method correlate well with more invasive and complex methods of detecting PAD.9, 10
The purpose of this study was to investigate whether atrial fibrillation influenced ABI measurement results. Accordingly, Doppler ABI measurements performed during atrial fibrillation were compared with ABI measurements performed in sinus rhythm.
Methods
Study design
A total of 115 consecutive patients with atrial fibrillation admitted for electrical cardioversion were screened by the Department of Internal Medicine, Hypertension and Vascular Diseases, Medical University of Warsaw (Figure 1). Participants were recruited to the study between October 2012 and December 2015. A total of 16 patients were excluded from the study due to failure to perform ABI measurement before cardioversion in 6 cases (the arteries were incompressible in 4 cases, and the investigator could not obtain a signal in 2 cases), withdrawal of consent after cardioversion (1 patient) and failure to maintain sinus rhythm after cardioversion (9 patients). A total of 99 patients (age 66.6±11 years, 63 males and 36 females) underwent the complete study protocol and were analyzed. Study population characteristics are presented in Table 1.
Exclusion criteria included circulatory instability, use of vasoconstrictive agents, limb trauma or upper limb artery stenosis. Neither participants nor those administering interventions or assessing study outcomes were blinded to study conditions or patient cardiac rhythm status. All study procedures were performed at the Department of Internal Medicine, Hypertension and Vascular Diseases, Medical University of Warsaw.
The study was accepted by the local bioethical committee, and informed consent was obtained from all participants. This trial was registered with ClinicalTrials.gov (NCT02986282).
Two separate study sessions were conducted before and after electrical cardioversion. The first session ended before propofol anesthesia was induced. The second session began in the same operating room with the patient fully conscious ∼1 h following cardioversion. Study procedures were performed within 2 h. All 99 patients underwent successful electrical cardioversion and both study sessions. No adverse events were observed.
ABI measurements
All measurements were performed in the intensive care unit at an ambient temperature of 21 °C shortly after written informed consent was obtained. All patients were awake, fasted and in the supine position. ABI was measured according to the AHA (American Heart Association) guidelines by either an investigator (MD) or a study nurse trained by the vascular department.6 SBP was measured using a Doppler device (Echo Sounder ES-101EX, Hadeco, Kawasaki, Japan) and a validated and calibrated aneroid sphygmomanometer (Minimus II, Riester, Jungingen, Germany). For each measurement, the appropriate cuff size was used, with the cuff width measuring at least 40% of the limb circumference. The arm with higher SBP and the higher SBP measured on the posterior tibial or dorsalis pedis artery was used to calculate the ABI. During both study sessions throughout the study, ABI measurements were repeated 3 times in an alternating clockwise (right arm, right popliteal, right dorsalis pedis, left popliteal, left dorsalis pedis, left arm, right arm) or counterclockwise sequence starting with the left arm, with each successive set of measurements taken in the reverse order. The same sequence of limb pressure measurements was used during the study. The measurements were repeated three times, and the mean measurement results were used for calculations. One investigator (MD), a study nurse trained at the vascular department, performed all ABI measurements.
End point
The primary end point of this study was the difference between ABI measurements before and after electrical cardioversion evaluated using comparison of central tendency measures and Bland–Altman plot inspection.
Statistical methods
Sample size calculations were based on preliminary observations made by the study team. The calculations showed that a sample size of 79 subjects would be needed to detect a 0.1 difference in ABI measured in sinus rhythm and during atrial fibrillation with a two-tailed α of 0.05 and a 1-β of 0.9. Our initial sample size estimate of 115 patients incorporated the assumption of attrition due to noneffective electrical cardioversion, patient decisions to quit the study or failure to obtain adequate ABI. Intraobserver variability was calculated using intraclass correlation coefficients.
Data were processed using a normality test (Shapiro–Wilk test). ABI in sinus rhythm and during atrial fibrillation were compared using the Wilcoxon signed-rank test. A paired two-tailed t-test was used for normal data distributions. The Bland–Altman plot was used to analyze agreement between ABI measurements performed in sinus rhythm (reference conditions) and during atrial fibrillation (experimental conditions). Correlations were analyzed between ABI measurements in sinus rhythm and those during atrial fibrillation, and Spearman’s rho coefficient was estimated. Statistical significance was established at P<0.05. Sensitivity and specificity for detection of PAD (ABI ⩽0.9) during atrial fibrillation were calculated. All data were calculated using R 3.1.3 statistical software (www.r-project.org) and were expressed as median (interquartile range) and mean values11 as appropriate.
Results
In the investigated population, 3 cases of PAD (ABI ⩽0.9) and 5 borderline PAD cases (ABI 0.91–1.0) were detected. The reference standard was the ABI measurement performed in sinus rhythm.
Restoration of sinus rhythm was associated with a significant decrease in heart rate from 101.9±23 to 64.3±8 beats per min, respectively (P<0.001).
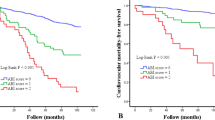
There was a statistically significant difference in the mean ABI during atrial fibrillation compared with sinus rhythm on both lower extremities (right: 1.132 (1.065–1.210) vs. 1.179 (1.080–1.242), respectively, P=0.019; left: 1.142 (1.075–1.222) vs. 1.170 (1.098–1.255), respectively, P=0.011) (Figure 2). The median ABI differences and confidence intervals (CIs) were 0.024 (95% CI: 0.004–0.045) and 0.022 (95% CI: 0.005–0.040) for the right and left sides, respectively.
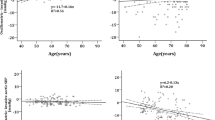
The Bland–Altman plot showed good agreement between Doppler method measurements during atrial fibrillation and in sinus rhythm (Figure 3). There was also a correlation between overall results during atrial fibrillation and in sinus rhythm (r=0.61, P<0.001 and r=0.67, P<0.001) for the right and left sides, respectively (Figure 4). Among the subgroup of patients with heart rates below 100 per min during atrial fibrillation (52 patients), the ABI was not significantly different before or after electrical cardioversion (right side: 1.145 (1.077–1.222) vs. 1.180 (1.087–1.240) respectively, P=0.350; left side: 1.170 (1.095–1.222) vs. 1.190 (1.110–1.260) respectively, P=0.414). Among the subgroup of patients with heart rates over 99 beats per min (47 patients) during atrial fibrillation, ABI was significantly different before and after electrical cardioversion (right side: 1.119 (1.055–1.190) vs. 1.190 (1.075–1.250) respectively, P=0.018; left side: 1.120 (1.030–1.211) vs. 1.164 (1.080–1.250) respectively, P=0.004).
Bland–Altman plot for the right (upper panel) and left (lower panel) side showing agreement between ankle–brachial index (ABI) measurements performed using the Doppler method during atrial fibrillation and in sinus rhythm. A full color version of this figure is available at the Hypertension Research journal online.
The single observer intraclass correlation coefficient was 0.93 (95% CI: 0.91–0.95) for measurements performed in sinus rhythm that differed from observations performed during atrial fibrillation (intraclass correlation coefficient=0.83; 95% CI: 0.79–0.86).
Discussion
To date, no reports exist concerning the impact of AF on ABI measurement accuracy using the reference Doppler method. Because the prevalence of atrial fibrillation and PAD increases with age,12, 13 it becomes more likely that patients will have symptoms or will not in be in sinus rhythm during PAD screening.
The main finding of the study is that the Doppler method ABI measurements during atrial fibrillation corresponded well with those in sinus rhythm. This finding was unexpected, as previous unpublished observations showed significant differences between ABI measurements during atrial fibrillation and sinus rhythm. However, those preliminary observations were based on nonrepeated measurements performed by different observers. In the current study, the authors analyzed the means of three ABI measurements. Furthermore, all measurements were performed by a single trained and experienced investigator. Good reproducibility of measurements was demonstrated, with a single observer intraclass correlation coefficient of 0.93 (95% CI: 0.91–0.95).
Repeated blood pressure measurements have been suggested for patients with atrial fibrillation to overcome variations in stroke volume.8, 14 Automated oscillometric measurements of blood pressure have shown satisfactory accuracy in determination of SBP in patients with atrial fibrillation.15, 16 Pagonas et al.17 found that systolic and diastolic blood pressure measurement biases did not significantly differ during atrial fibrillation in Bland–Altman analysis of oscillometric and invasive blood pressure measurements repeated 3 times. Other studies also showed that blood pressure measurements could be performed with satisfactory accuracy in patients with atrial fibrillation.18, 19 However, those studies analyzed only systolic and diastolic blood pressure, not ABI.
In our study, ABI measurements were repeated 3 times. Although it is a time-consuming method, other investigators have also used the mean of three measurements while evaluating blood pressure during atrial fibrillation.17, 20
In the current study, patients were evaluated before and after electrical cardioversion. This characteristic represents an important advantage of the study, as the protocol design enabled exact evaluation of the bias in ABI measurement related to the arrhythmia. In contrast to our study, previous investigations that assessed blood pressure variability during atrial fibrillation analyzed separate cohorts of subjects with atrial fibrillation and in sinus rhythm.17, 18, 19, 21
Comparison of ABI measurements before and after electrical cardioversion revealed a statistically significant difference. However, further analysis revealed that the upper bound of calculated CI for the median difference did not support statistical significance (P<0.05). Nonetheless, this low value of the upper bound of calculated CI strongly suggested that the observed median difference was clinically insignificant. This finding was confirmed by the results of Bland–Altman plot inspection that showed good agreement between measurements performed during atrial fibrillation and in sinus rhythm (Figure 3).
Notably, the analysis of the subgroup of patients with heart rates below 100 beats per min showed no difference in ABI during arrhythmia and in sinus rhythm compared with the group with atrial fibrillation >100 beats per min, among whom a difference was present. This finding suggests that ABI measurement was more prone to bias during atrial fibrillation with higher ventricular rates.
In the current study, PAD was detected in a small number of subjects. However, it must be emphasized that the study included consecutive patients admitted for electrical cardioversion rather than for PAD examination. A similar percentage of PAD subjects was also observed by other investigators in the general population.22 It would be interesting to include more patients already diagnosed with PAD in future studies. It is also noteworthy that this study was performed using the reference Doppler method performed by a single trained observer. As such, there was no interobserver variability and very good intraobserver reliability that may not be the case in real-life conditions.
In this study, higher blood pressure values were noted before electrical cardioversion (Table 2). The influence of arousal before the electrical cardioversion procedure must be taken into consideration, as the blood pressure-reducing action of the anesthetic would be less pronounced. However, because ABI is a ratio of blood pressures measured on arteries of the same caliber, increased blood pressure should affect both vascular beds similarly.
Additional analysis was performed while considering only the first measurements performed during atrial fibrillation and in sinus rhythm. No significant difference was detected between measurements obtained during atrial fibrillation and in sinus rhythm in the case of the left lower extremity. In contrast, a difference was detected, although judged to be clinically insignificant, when using repeated measurements. This finding strongly suggests that the accuracy of averaged repeated measurements is higher than that of a single measurement in subjects with atrial fibrillation. Furthermore, rho statistic values increased with the number of measurements, averaging between 0.46 and 0.56 for single right- and left-sided measurements, 0.56 and 0.6 for the average of two measurements and 0.61 and 0.67 for the average of three measurements, respectively. This finding also suggests that repeated measures may increase the measurement accuracy.
Conclusion
The results of this study show that atrial fibrillation does not have a clinically important effect on ABI measurements. This conclusion does not apply to other ABI measurement methods, such as the oscillometric method. Considering the study data, ABI evaluation should be performed using repeated measurements in patients with atrial fibrillation. Although this approach is time consuming, it is consistent with guidelines supporting averaged blood pressure measurements for patients with atrial fibrillation.8, 14
Further research of the population evaluated for PAD is needed because atrial fibrillation may cause more biased ABI results in subjects with lower ABI values.
References
Carter SA . Indirect systolic pressures and pulse waves in arterial occlusive diseases of the lower extremities. Circulation 1968; 37: 624–637.
Yao ST, Hobbs JT, Irvine WT . Ankle systolic pressure measurements in arterial disease affecting the lower extremities. Br J Surg 1969; 56: 676–679.
Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, Browner D . Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med 1992; 326: 381–386.
Saji N, Kimura K, Yagita Y, Kawarai T, Shimizu H, Kita Y . Comparison of arteriosclerotic indicators in patients with ischemic stroke: ankle-brachial index, brachial-ankle pulse wave velocity and cardio-ankle vascular index. Hypertens Res 2015; 38: 323–328.
Hashimoto T, Ichihashi S, Iwakoshi S, Kichikawa K . Combination of pulse volume recording (PVR) parameters and ankle-brachial index (ABI) improves diagnostic accuracy for peripheral arterial disease compared with ABI alone. Hypertens Res 2016; 39: 430–434.
Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, Fowkes FG, Hiatt WR, Jonsson B, Lacroix P, Marin B, McDermott MM, Norgren L, Pande RL, Preux PM, Stoffers HE, Treat-Jacobson D American Heart Association Council on Peripheral Vascular Disease Council on Epidemiology and Prevention Council on Clinical Cardiology Council on Cardiovascular Nursing Council on Cardiovascular Radiology and Intervention Council on Cardiovascular Surgery and Anesthesia. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation 2012; 126: 2890–2909.
Sykes D, Dewar R, Mohanaruban K, Donovan K, Nicklason F, Thomas DM, Fisher D . Measuring blood pressure in the elderly: does atrial fibrillation increase observer variability? BMJ 1990; 300: 162–163.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ . Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111: 697–716.
Guo X, Li J, Pang W, Zhao M, Luo Y, Sun Y, Hu D . Sensitivity and specificity of ankle-brachial index for detecting angiographic stenosis of peripheral arteries. Circ J 2008; 72: 605–610.
Niazi K, Khan TH, Easley KA . Diagnostic utility of the two methods of ankle brachial index in the detection of peripheral arterial disease of lower extremities. Catheter Cardiovasc Interv 2006; 68: 788–792.
Schubert C, Lambertz M, Nelesen RA, Bardwell W, Choi JB, Dimsdale JE . Effects of stress on heart rate complexity—a comparison between short-term and chronic stress. Biol Psychol 2009; 80: 325–332.
Criqui MH, Aboyans V . Epidemiology of peripheral artery disease. Circ Res 2015; 116: 1509–1526.
Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE . Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001; 285: 2370–2375.
Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O'Brien E, Ohkubo T, Padfield P, Palatini P, Pickering T, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G, ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens 2008; 26: 1505–1526.
Stergiou GS, Kollias A, Destounis A, Tzamouranis D . Automated blood pressure measurement in atrial fibrillation: a systematic review and meta-analysis. J Hypertens 2012; 30: 2074–2082.
Kollias A, Stergiou GS . Automated measurement of office, home and ambulatory blood pressure in atrial fibrillation. Clin Exp Pharmacol Physiol 2014; 41: 9–15.
Pagonas N, Schmidt S, Eysel J, Compton F, Hoffmann C, Seibert F, Hilpert J, Tschope C, Zidek W, Westhoff TH . Impact of atrial fibrillation on the accuracy of oscillometric blood pressure monitoring. Hypertension 2013; 62: 579–584.
Lip GY, Zarifis J, Beevers M, Beevers DG . Ambulatory blood pressure monitoring in atrial fibrillation. Am J Cardiol 1996; 78: 350–353.
Jani B, Bulpitt CJ, Rajkumar C . Blood pressure measurement in patients with rate controlled atrial fibrillation using mercury sphygmomanometer and Omron HEM-750CP deice in the clinic setting. J Hum Hypertens 2006; 20: 543–545.
Wang XX, Shuai W, Hong K, Xu J, Li JX, Li P, Cheng XS, Su H . How to evaluate BP measurements using the oscillometric method in atrial fibrillation: the value of pulse rate variation. Hypertens Res 2016; 39: 588–592.
Hsu PC, Lee WH, Chu CY, Lin TH, Su HM, Lee CS, Voon WC, Lai WT, Sheu SH . Heart rate significantly influences the relationship between atrial fibrillation and ankle-brachial index. J Cardiol 2015; 66: 143–147.
Davies JH, Williams EM . Automated plethysmographic measurement of the ankle-brachial index: a comparison with the doppler ultrasound method. Hypertens Res 2016; 39: 100–106.
Acknowledgements
This study was supported by the Medical University of Warsaw.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dąbrowski, M., Lewandowski, J., Abramczyk, P. et al. Atrial fibrillation does not affect ankle–brachial index measured using the Doppler method. Hypertens Res 41, 60–65 (2018). https://doi.org/10.1038/hr.2017.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.89
Keywords
This article is cited by
-
The impact of atrial fibrillation on accuracy of oscillometric blood pressure measurement: effect of ventricular rate
Hypertension Research (2020)
-
Can we accurately measure the ankle-brachial index in patients with atrial fibrillation?
Hypertension Research (2018)