Abstract
Introduction
The metabolically healthy obese (MHO) phenotype may express typical characteristics on long-term follow-up. Little is known about the initiation of this phenotypes and its future stability.
Aim
The Clinical Practice Research Datalink (CPRD) is a large-scale primary care database. The aim of this study was to assess the stability of, and evaluate the factors associated with a transition into an unhealthy outcome in, a MHO population in the UK.
Methods
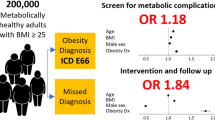
The CPRD was interrogated for a diagnosis of ‘obesity’ and cross-referenced with a body mass index (BMI) ≥35 kg/m2; participants were further classified as MH using a clinical diagnostic code or a relative therapeutic code. A hazard cox regression univariate and multivariate analysis evaluated the time to transition for independent variables.
Results
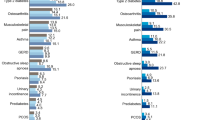
There were 231,399 patients with a recorded BMI of 35 kg/m2 or greater. Incomplete records were eliminated and follow-up limited to 300 months, the cohort was reduced to 180,560 patients. The prevalence of MHO within the obese population from the CPRD was 128,191/180,560 (71%). MHO individuals, who were of male gender (hazard ratio (HR) 1.23 (1.21–1.25), p = < 0.01), older age group (HR 3.93 (3.82–4.04), p = < 0.01), BMI of 50–60 kg/m2 at baseline (HR 1.32(1.26–1.38), p = 0.01), smokers (HR 1.07(1.05–1.09), p = < 0.01) and regionally from North West England (HR 1.15(1.09–1.21), p = < 0.01) were more prone to an unhealthy transition (to develop comorbidities). Overall, of those MH at baseline, 71,485/128,191(55.8%) remained healthy on follow-up, with a mean follow-up of 113.5 (standard deviations (SD) 78.6) months or 9.4 (SD 6.6) years.
Conclusions
From this unique large data set, there is a greater prevalence of MHO individuals in the UK population than in published literature elsewhere. Female gender, younger age group, and lower initial weight and BMI were found to be significant predictors of sustained metabolic health in this cohort. However, there remains a steady progressive transition from a healthy baseline over the years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organisation. Obesity and overweight. WHO factsheet 2018; www.who.int/mediacentre/factsheets/fs311/. Viewed 12 October 2017.
Phillips CM. Metabolically healthy obesity across the life course: epidemiology, determinants, and implications. Ann N Y Acad Sci. 2016:85–100. https://doi.org/10.1111/nyas.13230.
Bluher M. Are there still healthy obese patients? Curr Opin Endocrinol Diabetes Obes. 2012;19:341–6.
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 91 million participants. Lancet. 2011;377:557–67.
Wildman RP, Muntner P, Reynolds K, Mcginn AP. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering. Arch Intern Med. 2013;168:1617–24.
Phillips CM. Metabolically healthy obesity: definitions, determinants and clinical implications. Rev Endocr Metab Disord. 2013;14:219–27.
Ogorodnikova A, Kim M, McGinn A, Muntner P, Khan U, Wildman R, et al. Incident cardiovascular disease events in metabolically benign obese individuals. Obesity. 2012;20:651–9.
Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97:2482–8.
Bell JA, Kivimaki M, Hamer M. Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev. 2014;15:504–15.
Dalzill C, Nigam A, Juneau M, Guilbeault V, Latour E, Mauriège P, et al. Intensive lifestyle intervention improves cardiometabolic and exercise parameters in metabolically healthy obese and metabolically unhealthy obese individuals. Can J Cardiol. 2014;30:434–40.
Alam I, Ng TP, Larbi A. Does inflammation determine whether obesity is metabolically healthy or unhealthy? The aging perspective. Mediat Inflamm. 2012;2012:456456.
Aguilar-Salinas CA, García E, Robles L, Riaño D, Ruiz-Gomez DG, García-Ulloa AC, et al. High adiponectin concentrations are associated with the metabolically healthy obese phenotype. J Clin Endocrinol Metab. 2008;93:4075–9.
Meigs JB, Wilson PWF, Fox CS, Vasan RS, Nathan DM, Sullivan LM, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006;91:2906–12.
Lynch L, O’Connell JM, Kwasnik AK, Cawood TJ, O’Farrelly C, O’Shea DB. Are natural killer cells protecting the metabolically healthy obese patient? Obesity. 2009;17:601–5.
Williams T, van Staa T, Puri S, Eaton S. Recent advances in the utility and use of the General Practice Research Database as an example of a UK Primary Care Data resource. Ther Adv Drug Saf. 2012;3:89–99.
Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: A systematic review. Br J Clin Pharmacol. 2010;69:4–14.
Howell J. The General Practice Research Database: quality of morbidity data. Popul Trends. 1997;87:36–40.
Donegan K, Fox N, Black N, Livingston G, Banerjee S, Burns A. Trends in diagnosis and treatment for people with dementia in the UK from 2005 to 2015: a longitudinal retrospective cohort study. Lancet. 2017;2:e149–56.
Pascoe SW, Neal RD, Heywood PL, Allgar VL, Miles JN, Stefoski-Mikeljevic J. Identifying patients with a cancer diagnosis using general practice medical records and Cancer Registry data. Fam Pract. 2008;25:215–20.
Bhaskaran K, Douglas I, Forbes H, Dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: A population-based cohort study of 5·24 million UK adults. Lancet. 2014;384:755–65.
Nazareth I, King M, Haines A, Rangel L, Myers S. Accuracy of diagnosis of psychosis on general practice computer system. BMJ . 1993;307:32–4.
Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60:199–206.
Mathur R, Bhaskaran K, Chaturvedi N, Leon DA, Van Staa T, Grundy E, et al. Completeness and usability of ethnicity data in UK-based primary care and hospital databases. J Public Health. 2014;36:684–92.
Ogorodnikova AD, Kim M, McGinn AP, Muntner P, Khan U, Wildman RP. Incident cardiovascular disease events in metabolically benign obese individuals. Obesity. 2012;20:651–9.
Achilike I, Hazuda HP, Fowler SP, Lorenzo C, Antonio S. HHS public access. Int J Obes. 2015;39:228–34.
Hwang Y-C, Hayashi T, Fujimoto WY, Kahn SE, Leonetti DL, McNeely MJ, Boyko EJ. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int J Obes. 2016;19:69–77.
Soriguer F, Gutiérrez-Repiso C, Rubio-Martín E, García-Fuentes E, Almaraz MC, Colomo N, et al. Metabolically healthy but obese, a matter of time? Findings from the prospective pizarra study. J Clin Endocrinol Metab. 2013;98:2318–25.
Justicia J, Rosales A, Bañuel E, Oller-López JL, Valdivia M, Haïdour A, et al. Natural course of metabolically healthy overweight/obese subjects and the impact of weight change. J Clin Nurs. 2016;8:1–12.
Lassale C, Tzoulaki I, Moons KGM, Sweeting M, Boer J, Johnson L, et al. Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case-cohort analysis. Eur Heart J. 2018;39:397–406. https://doi.org/10.1093/eurheartj/ehx448.
Campbell J, Dedman DJ, Eaton SC, Gallagher AMWT. Is the CPRD GOLD population comparable to the UK population? Pharmacoepidemiol Drug Saf. 2013;22:280–1.
Herrett EL, Thomas SL, Smeeth L. Validity of diagnoses in the general practice research database. Br J Gen Pr. 2011;61:438–9.
Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, Staa Tvan, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol. 2015;44:827–36.
Funding
The authors have read the journal’s guidelines on finances and have no conflicts of interest to disclose. Word count: 3,172
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Moussa, O., Arhi, C., Ziprin, P. et al. Fate of the metabolically healthy obese—is this term a misnomer? A study from the Clinical Practice Research Datalink. Int J Obes 43, 1093–1101 (2019). https://doi.org/10.1038/s41366-018-0096-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0096-z