Abstract
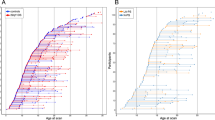
Low hippocampal volume is a consistent finding in schizophrenia and across the psychosis spectrum. However, there is a lack of studies investigating longitudinal hippocampal development and its relationship with psychotic symptoms. The 22q11.2 deletion syndrome (22q11DS) has proven to be a remarkable model for the prospective study of individuals at high risk of schizophrenia to unravel the pathophysiological processes predating the onset of psychosis. Repeated cerebral MRIs were acquired from 140 patients with 22q11DS (53 experiencing moderate-to-severe psychotic symptoms) and 135 healthy controls aged from 6 to 35 years and with up to 5 time points per participant. Hippocampal subfield analysis was conducted using FreeSurfer-v.6 and FIRST-FSL. Then, whole hippocampal and subfield volumes were compared across the groups. Relative to controls, patients with 22q11DS showed a remarkably lower volume of all subfields except for CA2/3. No divergent trajectories in hippocampal development were found. When comparing patients with 22q11DS exhibiting psychotic symptoms to those without psychosis, we detected a volume decrease during late adolescence, starting in CA1 and spreading to other subfields. Our findings suggested that hippocampal volume is consistently smaller in patients with 22q11DS. Moreover, we have demonstrated that patients with 22q11DS and psychotic symptoms undergo a further decrease in volume during adolescence, a vulnerable period for the emergence of psychosis. Interestingly, CA2/3, despite being affected in patients with psychotic symptoms, was the only area not reduced in patients with 22q11DS relative to controls, thus suggesting that its atrophy exclusively correlates with the presence of positive psychotic symptoms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Code availability
The code employed to model hippocampal developmental trajectories is available upon request.
References
Zeidman P, Maguire EA. Anterior hippocampus: The anatomy of perception, imagination and episodic memory. Nat Rev Neurosci. 2016;17:173–82.
Ota M, Sato N, Hidese S, Teraishi T, Maikusa N, Matsuda H, et al. Structural differences in hippocampal subfields among schizophrenia patients, major depressive disorder patients, and healthy subjects. Psychiatry Res Neuroimaging. 2017;259:54–9.
Haukvik UK, Tamnes CK, Söderman E, Agartz I. Neuroimaging hippocampal subfields in schizophrenia and bipolar disorder: A systematic review and meta-analysis. 2018;104:217–26.
Arnold SJM, Ivleva EI, Gopal TA, Reddy AP, Jeon-Slaughter H, Sacco CB, et al. Hippocampal volume is reduced in schizophrenia and schizoaffective disorder but not in psychotic bipolar i disorder demonstrated by both manual tracing and automated parcellation (FreeSurfer). Schizophr Bull. 2015;41:233–49.
Haijma SV, Van Haren N, Cahn W, Koolschiin PCMP, Hulshoff PHE, Kahn RS. Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects. Schizophr Bull. 2013;39:1129–38.
Van Erp TGM, Hibar DP, Rasmussen JM, Glahn DC, Pearlson GD, Andreassen OA, et al. Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Mol Psychiatry. 2016;21:547–53.
McHugo M, Talati P, Woodward ND, Armstrong K, Blackford JU, Heckers S. Regionally specific volume deficits along the hippocampal long axis in early and chronic psychosis. NeuroImage Clin. 2018;20:1106–14.
Falkai P, Malchow B, Wetzestein K, Nowastowski V, Bernstein HG, Steiner J, et al. Decreased oligodendrocyte and neuron number in anterior hippocampal areas and the entire hippocampus in schizophrenia: a stereological postmortem study. Schizophr Bull. 2016;42:S4–12.
Zaidel DW, Esiri MM, Harrison PJ. Size, shape, and orientation of neurons in the left and right hippocampus: Investigation of normal asymmetries and alterations in schizophrenia. Am J Psychiatry. 1997;154:812–8.
Vargas T, Dean DJ, Osborne KJ, Gupta T, Ristanovic I, Ozturk S, et al. Hippocampal subregions across the psychosis spectrum. Schizophr Bull. 2017;44:1091–9.
Nakahara S, Matsumoto M, van Erp TGM Hippocampal subregion abnormalities in schizophrenia: a systematic review of structural and physiological imaging studies. Neuropsychopharmacol Rep. 2018;38:156–66.
Baglivo V, Cao B, Mwangi B, Bellani M, Perlini C, Lasalvia A, et al. Hippocampal subfield volumes in patients with first-episode psychosis. Schizophr Bull. 2018;44:552–9.
Sauras R, Keymer A, Alonso-Solis A, Díaz A, Molins C, Nuñez F, et al. Volumetric and morphological characteristics of the hippocampus are associated with progression to schizophrenia in patients with first-episode psychosis. Eur Psychiatry. 2017;45:1–5.
Dean DJ, Orr JM, Bernard JA, Gupta T, Pelletier-Baldelli A, Carol EE, et al. Hippocampal shape abnormalities predict symptom progression in neuroleptic-free youth at ultrahigh risk for psychosis. Schizophr Bull. 2016;42:161–9.
Harrisberger F, Buechler R, Smieskova R, Lenz C, Walter A, Egloff L, et al. Alterations in the hippocampus and thalamus in individuals at high risk for psychosis. npj Schizophr. 2016;2:16033.
Walter A, Suenderhauf C, Harrisberger F, Lenz C, Smieskova R, Chung Y, et al. Hippocampal volume in subjects at clinical high-risk for psychosis: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2016;71:680–90.
Kawano M, Sawada K, Shimodera S, Ogawa Y, Kariya S, Lang DJ, et al. Hippocampal subfield volumes in first episode and chronic schizophrenia. PLoS ONE. 2015;10:e0117785.
Ho NF, Iglesias JE, Sum MY, Kuswanto CN, Sitoh YY, De Souza J, et al. Progression from selective to general involvement of hippocampal subfields in schizophrenia. Mol Psychiatry. 2017;22:142–52.
Small SA, Schobel SA, Buxton RB, Witter MP, Barnes CA. A pathophysiological framework of hippocampal dysfunction in ageing and disease Scott. Nat Rev Neurosci. 2012;12:585–601.
Mizuseki K, Royer S, Diba K, Buzsáki G. Activity dynamics and behavioral correlates of CA3 and CA1 hippocampal pyramidal neurons. 2013;22:1659–80.
Cenquizca LA, Swanson LW. Spatial organization of direct hippocampal field CA1 axonal projections to the rest of the cerebral cortex. Brain Res Rev. 2007;56:1–26.
Knierim JJ. The hippocampus. Current Biology. 2015;25:R1116–21.
Eichenbaum H. A cortical—hippocampal system for declarative memory. 2000;1:1–10.
Talati P, Rane S, Kose S, Blackford JU, Gore J, Donahue MJ, et al. Increased hippocampal CA1 cerebral blood volume in schizophrenia. NeuroImage Clin. 2014;5:359–64.
Behrendt RP. Contribution of hippocampal region CA3 to consciousness and schizophrenic hallucinations. Neurosci Biobehav Rev [Internet]. 2010;34:1121–36.
Marr D. Simple memory: a theory for archicortex. Philos Trans R Soc Lond B Biol Sci. 1971;262:23–81.
Tamminga CA, Stan AD, Wagner AD. The hippocampal formation in schizophrenia. Am J Psychiatry. 2010;167:1178–93.
Lieberman JA, Girgis RR, Brucato G, Moore H, Provenzano F, Kegeles L, et al. Hippocampal dysfunction in the pathophysiology of schizophrenia: a selective review and hypothesis for early detection and intervention. Mol Psychiatry. 2018. http://www.nature.com/doifinder/10.1038/mp.2017.249.
Ho NF, Holt DJ, Cheung M, Iglesias JE, Goh A, Wang M, et al. Progressive decline in hippocampal CA1 volume in individuals at ultra-high-risk for psychosis who do not remit: findings from the longitudinal youth at risk study. Neuropsychopharmacology. 2017;42:1361–70.
Schobel SA, Chaudhury NH, Khan UA, Paniagua B, Styner MA, Asllani I, et al. Imaging patients with psychosis and a mouse model establishes a spreading pattern of hippocampal dysfunction and implicates glutamate as a driver. Neuron. 2013;78:81–93.
Abele AE, Scholz KP, Scholz WK, Miller RJ. Excitotoxicity induced by enhanced excitatory neurotransmission in cultured hippocampal pyramidal neurons. Neuron. 1990;4:413–9.
Ho BC, Magnotta V. Hippocampal volume deficits and shape deformities in young biological relatives of schizophrenia probands. Neuroimage. 2010;49:3385–93.
Keshavan MS, Dick E, Mankowski I, Harenski K, Montrose DM, Diwadkar V, et al. Decreased left amygdala and hippocampal volumes in young offspring at risk for schizophrenia. Schizophr Res. 2002;58:173–83.
Hill K, Bolo N, Sarvode Mothi S, Lizano P, Guimond S, Tandon N, et al. Subcortical surface shape in youth at familial high risk for schizophrenia. Psychiatry Res Neuroimaging. 2017;267:36–44.
Tepest R, Wang L, Miller MI, Falkai P, Csernansky JG. Hippocampal deformities in the unaffected siblings of schizophrenia subjects. Biol Psychiatry. 2003;54:1234–40.
Johnson SLM, Wang L, Alpert KI, Greenstein D, Clasen L, Lalonde F, et al. Hippocampal shape abnormalities of patients with childhood-onset schizophrenia and their unaffected siblings. J Am Acad Child Adolesc Psychiatry. 2013;52:527–536.e2.
Whelan CD, Hibar DP, Van Velzen LS, Zannas AS, Carrillo-Roa T, McMahon KZ, et al. Heritability and reliability of automatically segmented human hippocampal formation subregions. Neuroimage. 2016;128:125–37.
Dutt A, McDonald C, Dempster E, Prata D, Shaikh M, Williams I, et al. The effect of COMT, BDNF, 5-HTT, NRG1 and DTNBP1 genes on hippocampal and lateral ventricular volume in psychosis. Psychol Med. 2009;39:1783–97.
Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rössler A, Schultze-Lutter F, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. Arch Gen Psychiatry. 2013;70:107–20.
McGuffin P, Owen MJ, Farmer AE. Genetic basis of schizophrenia. Lancet. 1995;346:678–82.
Maude Schneider, Martin Debbanè, Anne Bassett, Psychiatric SCEW. Disorders from childhood to adulthood in 22q11.2 deletion syndrome: results from the international consortium on brain and behavior in 22q11.2. Deletion Syndrome Maude. 2015;171:627–39.
Schneider M, Armando M, Pontillo M, Vicari S, Debbané M, Schultze-Lutter F, et al. Ultra high risk status and transition to psychosis in 22q11.2 deletion syndrome. World Psychiatry. 2016;15:259–65.
Jonas RK, Montojo CA, Bearden CE. The 22q11.2 deletion syndrome as a window into complex neuropsychiatric disorders over the lifespan. Biol Psychiatry. 2014;75:351–60.
Eliez S, Schmitt JE, White CD, Reiss AL. Children and adolescents with velocardiofacial syndrome: A Volumetric MRI Study. Am J Psychiatry. 2000;157:409–15.
Schaer M, Eric Schmitt J, Glaser B, Lazeyras F, Delavelle J, Eliez S. Abnormal patterns of cortical gyrification in velo-cardio-facial syndrome (deletion 22q11.2): an MRI study. Psychiatry Res Neuroimaging. 2006;146:1–11.
Scott JA, Goodrich-Hunsaker N, Kalish K, Lee A, Hunsaker MR, Schumann CM, et al. The hippocampi of children with chromosome 22q11.2 deletion syndrome have localized anterior alterations that predict severity of anxiety. J Psychiatry Neurosci. 2016;41:203–13.
Eliez S, Blasey CM, Ph D, Schmitt EJ, White CD, Hu D, et al. Velocardiofacial syndrome: are structural changes in the temporal and mesial temporal regions related to schizophrenia? Am J Psychiatry. 2001;158:447–53.
Debbané M, Schaer M, Farhoumand R, Glaser B, Eliez S. Hippocampal volume reduction in 22q11.2 deletion syndrome. Neuropsychologia. 2006;44:2360–5.
Flahault A, Schaer M, Ottet MC, Debbané M, Eliez S. Hippocampal volume reduction in chromosome 22q11.2 deletion syndrome (22q11.2DS): A longitudinal study of morphometry and symptomatology. Psychiatry Res Neuroimaging. 2012;203:1–5.
DeBoer T, Wu Z, Lee A, Simon TJ. Hippocampal volume reduction in children with chromosome 22q11.2 deletion syndrome is associated with cognitive impairment. Behav Brain Funct. 2007;3:1–9.
Iglesias JE, Augustinack JC, Nguyen K, Player CM, Player A, Wright M, et al. A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: application to adaptive segmentation of in vivo MRI. Neuroimage. 2015;115:117–37.
Van Leemput K, Bakkour A, Benner T, Wiggins G, Wald LL, Augustinack J, et al. Automated segmentation of hippocampal subfields from ultra-high resolution in vivo MRI. Hippocampus. 2009;19:549–57.
Csernansky JG, Wang L, Ph D, Posener JA, Heydebrand G, Ph D, et al. Hippocampal deformities in schizophrenia characterized by high dimensional brain mapping. Am J Psychiatry. 2002;159:2000–6.
Patenaude B, Smith SM, Kennedy D, Jenkinson M. A Bayesian model of shape and appearance for subcortical brain segmentation. Neuroimage. 2012;56:907–22.
Debbané M, Glaser B, David MK, Feinstein C, Eliez S. Psychotic symptoms in children and adolescents with 22q11.2 deletion syndrome: Neuropsychological and behavioral implications. Schizophr Res. 2006;84:187–93.
Weisman O, Guri Y, Gur RE, McDonald-McGinn DM, Calkins ME, Tang SX, et al. Subthreshold psychosis in 22q11.2 deletion syndrome: Multisite naturalistic study. Schizophr Bull. 2017;43:1079–89.
Tang SX, Yi JJ, Moore TM, Calkins ME, Kohler CG, Whinna DA, et al. Subthreshold psychotic symptoms in 22q11.2 deletion syndrome. J Am Acad Child Adolesc Psychiatry [Internet]. 2014;53:991–1000.e2.
Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: Preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–5.
Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, et al. Whole brain segmentation: Automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33:341–55.
Dedrick RF, Ferron JM, Hess MR, Hogarty KY, Kromrey JD, Lang TR, et al. Multilevel modeling: a review of methodological issues and applications. Rev Educ Res. 2009;79:69–102.
Mutlu AK, Schneider M, Debbané M, Badoud D, Eliez S, Schaer M. Sex differences in thickness, and folding developments throughout the cortex. Neuroimage. 2013;82:200–7.
Franchini M, Zo D, Ms C, Gentaz E, Glaser B, Wilde HW De, et al. Early adaptive functioning trajectories in preschoolers with autism spectrum disorders. PLoS ONE. 2018;12:e0178859.
Krogsrud SK, Tamnes CK, Fjell AM, Amlien I, Grydeland H, Sulutvedt U, et al. Development of hippocampal subfield volumes from 4 to 22 years. Hum Brain Mapp. 2014;35:5646–57.
Fountain DM, Schaer M, Mutlu AK, Schneider M, Debbané M, Eliez S. Congenital heart disease is associated with reduced cortical and hippocampal volume in patients with 22q11.2 deletion syndrome. Cortex. 2014;57:128–42.
Tatu L, Vuillier F. Structure and vascularization of the human hippocampus. Hippocampus Clin Neurosci. 2014;34:18–25.
Chow EWC, Mikulis DJ, Zipursky RB, Scutt LE, Weksberg R, Bassett AS. Qualitative MRI findings in adults with 22q11 deletion syndrome and schizophrenia. 2012;46:1436–42.
Uematsu A, Matsui M, Tanaka C, Takahashi T, Noguchi K, Suzuki M, et al. Developmental trajectories of amygdala and hippocampus from infancy to early adulthood in healthy individuals. PLoS ONE. 2012;7:1–10.
Knickmeyer RC, Gouttard S, Kang C, Evans D, Smith JK, Hamer RM, et al. A structural MRI study of human brain development from birth to 2 years. J Neurosci. 2010;28:12176–82.
Nitin G, Tom FN, Herman DH, Ordonez A, Greenstein D, Hayashi KM, et al. Dynamic mapping of normal human hippocampal development. Hippocampus. 2007;17:801–12.
Sorrells SF, Paredes MF, Cebrian-Silla A, Sandoval K, Qi D, Kelley KW, et al. Human hippocampal neurogenesis drops sharply in children to undetectable levels in adults. Nature. 2018;555:377–81.
Molinard-Chenu A, Dayer A. The candidate schizophrenia risk gene DGCR2 regulates early steps of corticogenesis. Biol Psychiatry. 2018;83:692–706.
Flore G, Cioffi S, Bilio M, Illingworth E. Cortical development requires mesodermal expression of Tbx1, a gene haploinsufficient in 22q11.2 deletion syndrome. Cereb Cortex. 2016. https://doi.org/10.1093/cercor/bhw076.
Donofrio MT, Bremer YA, Schieken RM, Gennings C, Morton LD, Eidem BW, et al. Autoregulation of cerebral blood flow in fetuses with congenital heart disease: The brain sparing effect. Pediatr Cardiol. 2003;24:436–43.
Kuhn S, Musso F, Mobascher A, Warbrick T, Winterer G, Gallinat J. Hippocampal subfields predict positive symptoms in schizophrenia: first evidence from brain morphometry. Transl Psychiatry. 2012;2:e127.
Mathew I, Gardin TM, Tandon N, Eack S, Francis AN, Seidman LJ, et al. Medial temporal lobe structures and hippocampal subfields in psychotic disorders: findings from the bipolar-schizophrenia network on intermediate phenotypes (B-SNIP) study. JAMA Psychiatry. 2014;71:769–77.
Zierhut KC, Graßmann R, Kaufmann J, Steiner J, Bogerts B, Schiltz K. Hippocampal CA1 deformity is related to symptom severity and antipsychotic dosage in schizophrenia. Brain. 2013;136:804–14.
Kalmady SV, Shivakumar V, Arasappa R, Subramaniam A, Gautham S, Venkatasubramanian G, et al. Clinical correlates of hippocampus volume and shape in antipsychotic-naïve schizophrenia. Psychiatry Res Neuroimaging. 2017;263:93–102.
Haukvik UK, Westlye LT, Mørch-Johnsen L, Jørgensen KN, Lange EH, Dale AM, et al. In vivo hippocampal subfield volumes in schizophrenia and bipolar disorder. Biol Psychiatry. 2015;77:581–8.
Bakker A, Kirwan CB, Miller M, Stark CEL. Pattern separation in the human hippocampal CA3 and dentate gyrus. Science. 2010;319:1640–2.
Li W, Ghose S, Gleason K, Begovic A, Perez J, Bartko J, et al. Synaptic proteins in the hippocampus indicative of increased neuronal activity in CA3 in schizophrenia. Am J Psychiatry. 2015;172:373–82.
Tamminga CA, Southcott S, Sacco C, Wagner AD, Ghose S. Glutamate dysfunction in hippocampus: Relevance of dentate gyrus and CA3 signaling. Schizophr Bull. 2012;38:927–35.
Kraguljac NV, Carle M, Frölich MA, Tran S, Yassa MA, White DM, et al. Mnemonic discrimination deficits in first-episode psychosis and a ketamine model suggests dentate gyrus pathology linked to N-methyl-D-aspartate receptor hypofunction. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3:231–8.
Das T, Ivleva EI, Wagner AD, Stark CEL and Tamminga CA. Loss of pattern separation performance in schizophrenia suggests dentate gyrus dysfunction. Schizophr Res. 2014;159:193–7.
Martinelli C, Shergill SS. Clarifying the role of pattern separation in schizophrenia: The role of recognition and visual discrimination de fi cits. Schizophr Res. 2015;166:328–33.
Schobel SA, Lewandowski NM, Corcoran CM, Moore H, Brown T, Malaspina D, et al. Differential targeting of the CA1 subfield of the hippocampal formation by schizophrenia and related psychotic disorders. Arch Gen Psychiatry. 2009;66:938–46.
Lenka A, Ingalhalikar M, Shah A, Saini J, Arumugham SS, Hegde S, et al. Hippocampal subfield atrophy in patients with Parkinson’s disease and psychosis. J Neural Transm. 2018;0:1–12.
Kumral E, Deveci EE, Erdoʇan CE, Enüstün C. Isolated hippocampal infarcts: Vascular and neuropsychological findings. J Neurol Sci. 2015;356:83–9.
Weis S, Haug H, Holoubek B, Orün H. The cerebral dominances: quantitative morphology of the human cerebral cortex. Int J Neurosci. 1989;47:165–8.
Utsunomiya H, Takano K, Okazaki M, Mitsudome A. Development of the temporal lobe in infants and children: analysis by MR-based volumetry. Am J Neuroradiol. 1999;20:717–23.
Thompson DK, Wood SJ, Doyle LW, Warfield SK, Egan GF, Inder TE. MR-determined hippocampal asymmetry in full-term and preterm neonates. Hippocampus. 2009;19:118–23.
Okada N, Fukunaga M, Yamashita F, Koshiyama D, Yamamori H, Ohi K, et al. Abnormal asymmetries in subcortical brain volume in schizophrenia. Mol Psychiatry. 2016;21:1460–6.
Giedd JN, Vaituzis AC, Hamburger SD, Lange N, Rajapakse JC, Kaysen D, et al. Quantitative MRI of the temporal lobe, amygdala, and hippocampus in normal human development: ages 4–18 years. J Comp Neurol. 1996;366:223–30.
De Almeida JR, James AL, Papsin BC, Weksburg R, Clark H, Blaser S. Thyroid gland and carotid artery anomalies in 22qll.2 deletion syndromes. Laryngoscope. 2009;119:1495–500.
Heilbronner U, Samara M, Leucht S, Falkai P, Schulze TG. The Longitudinal Course of Schizophrenia Across the Lifespan: Clinical, Cognitive, and Neurobiological Aspects. 2016;24: 118–28.
Gothelf D, Schneider M, Green T, Debbané M, Frisch A, Glaser B, et al. Risk factors and the evolution of psychosis in 22q11.2 deletion syndrome: a longitudinal 2-site study. J Am Acad Child Adolesc Psychiatry. 2013;52:17–25.
Kraguljac NV, White DM, Reid MA, Lahti AC. Increased hippocampal glutamate and volumetric deficits in unmedicated patients with schizophrenia. JAMA Psychiatry. 2013;70:1294–302.
da Silva Alves F, Boot E, Schmitz N, Nederveen A, Vorstman J, Lavini C, et al. Proton magnetic resonance spectroscopy in 22q11 deletion syndrome. PLoS ONE. 2011;6:1–7.
Phillips LJ, McGorry PD, Garner B, Thompson KN, Pantelis C, Wood SJ, et al. Stress, the hippocampus and the hypothalamic-pituitary-adrenal axis: Implications for the development of psychotic disorders. Aust N Z J Psychiatry. 2006;40:725–41.
Vergaelen E, Schiweck C, Van Steeland K, Counotte J, Veling W, Swillen A, et al. A pilot study on immuno-psychiatry in the 22q11.2 deletion syndrome: a role for Th17 cells in psychosis? Brain Behav Immun. 2018;70:88–95.
Li W, Li K, Guan P, Chen Y, Xiao Y, Lui S, et al. NeuroImage: clinical volume alteration of hippocampal sub fi elds in fi rst-episode antipsychotic- naïve schizophrenia patients before and after acute antipsychotic treatment. NeuroImage Clin. 2018;20:169–76.
Acknowledgements
We would like to thank all the families who contributed to the study, as well as the family associations (Génération 22, Connect 22, Relais 22) for their ongoing support. Special thanks go to Léa Chambaz and Virginie Pouillard for coordinating the project and to the MRI operators at the Center of Biomedical Imaging (CIBM), François Lazeyras, Lydia Dubourg, Maëlle Chambaz, Laura Juan Galmes, and Joëlle van der Molen for their help in scanning.
Funding
This work was supported by research grants from the Swiss National Science Foundation (grant numbers 324730_121996, 324730_144260 to SE) and The National Centre of Competence in Research (NCCR) “Synapsy—The Synaptic Bases of Mental Diseases” (grant number 51NF40-158776 to SE). Personal grants by the Swiss National Science Foundation (grant numbers PZ00P1_174206 to M.Schn. and 163859 to M.Scha.) also supported the present work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mancini, V., Sandini, C., Padula, M.C. et al. Positive psychotic symptoms are associated with divergent developmental trajectories of hippocampal volume during late adolescence in patients with 22q11DS. Mol Psychiatry 25, 2844–2859 (2020). https://doi.org/10.1038/s41380-019-0443-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-019-0443-z
This article is cited by
-
Amygdala subdivisions exhibit aberrant whole-brain functional connectivity in relation to stress intolerance and psychotic symptoms in 22q11.2DS
Translational Psychiatry (2023)
-
Trajectories of imitation skills in preschoolers with autism spectrum disorders
Journal of Neurodevelopmental Disorders (2022)
-
Contribution of schizophrenia polygenic burden to longitudinal phenotypic variance in 22q11.2 deletion syndrome
Molecular Psychiatry (2022)
-
Long-term effects of early treatment with SSRIs on cognition and brain development in individuals with 22q11.2 deletion syndrome
Translational Psychiatry (2021)
-
Hippocampal regenerative medicine: neurogenic implications for addiction and mental disorders
Experimental & Molecular Medicine (2021)